Covid-19: How safe are the corona vaccines?
Updated onChristiane Fux studied journalism and psychology in Hamburg. The experienced medical editor has been writing magazine articles, news and factual texts on all conceivable health topics since 2001. In addition to her work for, Christiane Fux is also active in prose. Her first crime novel was published in 2012, and she also writes, designs and publishes her own crime plays.
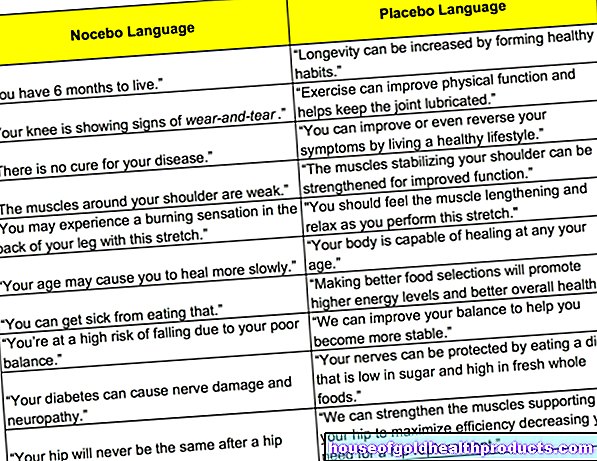
More posts by Christiane Fux All content is checked by medical journalists.Almost a year after the discovery of the new Sars-CoV-2 virus, the first vaccine was approved in the EU - a record. Before that, it took ten years and more to do this. Read here how this can be done so quickly without jeopardizing the safety of the vaccination and how safe the novel gene-based vaccines are in principle.

What does the use of gene-based vaccines mean?
The vaccines approved so far in the EU are mRNA or vector vaccines. Some people worry because these are novel, gene-based vaccines.
In fact, these mRNA vaccines are the first of their kind to be used to vaccinate humans. However, development of this type of vaccine began years ago - so they are not as new as it seems. Vector vaccines have also only recently been used.
However, worries that they could alter the genetic makeup and thus cause cancer, for example, are unfounded. Although the mRNA that is channeled into the body cells is a segment of the virus genome, it cannot be incorporated into the differently designed human DNA genome.
Basically the same thing happens with an mRNA vaccination as with an infection. The only difference is that instead of the dangerous virus, only a harmless surface protein triggers the vaccination reaction. Read more about mRNA vaccines here.
In the case of vector vaccines, on the other hand, a section of DNA actually gets into the nucleus of the vaccinated cell, where it is first converted into RNA. However, it is extremely unlikely that this gene segment will be incorporated into human DNA. They lack certain tools that could help them do this. In addition, the cells that come into contact with the vaccination quickly perish. This means that your cell nucleus is also broken down by the body.
Read more about vector vaccines here.
Better tolerated than classic vaccines?
In fact, mRNA vaccines could prove to be particularly well-tolerated: They contain only the bare essentials that are needed for a vaccination reaction: a single mRNA snippet surrounded by a layer of fat. Vaccination boosters, so-called adjuvants, such as those contained in many vaccines, are not necessary, for example. These are not well tolerated by some people.
What are the known side effects?
Millions of people around the world have now been vaccinated with the vaccines. Serious side effects that went beyond the usual flu-like vaccination reactions such as fever, muscle pain or headache were observed only in rare cases. Including very rare cerebral vein thromboses from the AstraZeneca vaccine.
Read more about vaccination reactions and complications here.
Mild side effects more common than usual
For the mRNA vaccines from BioNTech / Pfizer and Moderna, it has been found that the body, which has already prepared itself against the antigens after the first vaccination, then reacts more strongly - with fever, headache, fatigue. This is a sign that the vaccination has triggered an appropriate immune response in the body.
With the vector vaccine from AstraZeneca, on the other hand, the first vaccination is usually associated with stronger vaccination reactions.
Why was it able to develop so quickly?
While most people are relieved that the end of the pandemic is nearing thanks to vaccines, others worry that the rapid development may have come at the expense of safety. But that is not the case.
In fact, there are a number of factors that could significantly speed up vaccine development - without taking any risks.
Development builds on previous research
Vaccine development didn't have to start from scratch. It was able to build on knowledge that had already been gathered during vaccine research for other coronaviruses closely related to Sars-CoV-2: the Sars virus from 2002 and the MERS coronavirus.
It was therefore already known, for example, that the spike protein, which sits on the surface of coronaviruses, is suitable as a so-called antigen. With this protein, which is typical for viruses, the immune system can be prepared for defense against the virus. Finding such an antigen takes a lot of time. In fact, the two vaccines currently being approved are based on exactly this spike protein.
How have bureaucratic processes been accelerated?
In view of the urgency, the bureaucratic processes that have to be followed for the development and approval of a vaccine have been given high priority, made more effective and thus considerably accelerated. Even the applications for the studies were checked and granted with high priority.
A so-called rolling review process was used for approval. This means that not all data was first collected and then presented to the authorities after all studies were completed, but the data was submitted gradually. In this way, the authorities were able to start testing much earlier and request any data that was still required directly from the manufacturers.
Time was also saved in other areas: The financing of the vaccines was unproblematic in view of the pandemic. Otherwise, it takes a lot of time to set this up. The recruiting of test subjects for the studies was also carried out very quickly - enough volunteers registered quickly.
Faster production than classic vaccines
Another decisive factor: the production routes are many times faster than with classic vaccines. For this, viral material must first be cultivated in millions of chicken eggs, which is laborious and time-consuming. With the new vaccines, only a rapidly reproducible section of the genome is required. The human body cells then take over the production of the vaccine themselves.
High security after millions of people have been vaccinated
Despite all the precautionary measures, there is no 100 percent security - neither with this vaccination nor with vaccinations that took longer to develop.
After the corona vaccines have already been inoculated millions of times around the world, the safety of these vaccines is now much higher than that of many other, older vaccines. Very rare side effects were discovered that are only noticeable when not only tens of thousands, but hundreds of thousands or millions of people have been vaccinated. That is exactly the case here now.
Side effects that occur late are also unlikely to occur. Vaccination complications usually occur shortly after the vaccinations, at most after a few months. After so much time has passed since vaccination started around the world, such side effects must have occurred long ago.
Report side effects - and respond to them
Indications of serious side effects are immediately taken into account for the vaccination strategy. For example, after rare cerebral vein thromboses were observed in younger people who were vaccinated after the administration of AstraZeneca, in Germany it is only vaccinated in people aged 60 and over.
Confidence in vaccine safety is the cornerstone of a successful corona vaccination campaign. In order to ensure transparency and clarification, you have the option of reporting any suspected side effects following a corona vaccination to official bodies.
One possibility is to report such a suspected adverse effect using the Paul Ehrlich Institute's online form.
Please note: If you experience unwanted vaccination reactions after a corona vaccination, you should contact a doctor immediately.
Tags: womenshealth Diseases diet
















.jpg)


.jpg)