Polymyositis
and Sabine Schrör, medical journalistMarian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the expertsSabine Schrör is a freelance writer for the medical team. She studied business administration and public relations in Cologne. As a freelance editor, she has been at home in a wide variety of industries for more than 15 years. Health is one of her favorite subjects.
More about the experts All content is checked by medical journalists.Polymyositis is a rare inflammatory muscle disease. It is similar to dermatomyositis, but does not cause any changes to the skin. The symptoms in the muscles, on the other hand, cover the same spectrum, so muscle weakness and pain are in the foreground. Find out everything you need to know about polymyositis here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M33

Brief overview
- Definition: Polymyositis is a rare inflammatory muscle disease belonging to the group of rheumatic diseases. It mainly affects adult women.
- Symptoms: fatigue, general weakness, fever, muscle weakness (especially in the shoulder and pelvic area), muscle pain, joint pain, possibly other symptoms (e.g. swallowing disorders, breathing problems, Raynaud's syndrome, swollen gums)
- Causes: Autoimmune disease, the cause of which is not fully understood. Presumably genetic and triggered by external factors (such as infections).
- Diagnosis: blood tests, electromyography (EMG), ultrasound, magnetic resonance imaging, muscle biopsy.
- Treatment: medication (cortisone, immunosuppressants), physiotherapy and targeted muscle training.
- Prognosis: The right treatment can usually significantly alleviate the symptoms or eliminate them completely. Often, however, a slight muscle weakness remains. Complications and accompanying tumor diseases can worsen the prognosis.
Polymyositis: definition and frequency
The term "polymyositis" comes from the Greek and describes an inflammation ("-itis") of many ("poly") muscles ("myos"). Polymyositis is a rheumatic disease and is very similar to dermatomyositis. Unlike these, however, it only affects the muscles and not the skin as well.
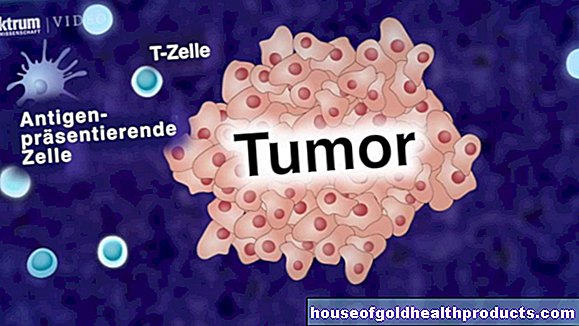
Both polymyositis and dermatomyositis are often associated with other diseases, such as other autoimmune diseases, viral infections, or cancer. A malignant tumor occurs much less often in polymyositis patients than in dermatomyositis patients.
With around five to ten new cases per million people per year worldwide, polymyositis is even less common than dermatomyositis. It almost exclusively affects adults, mostly between the ages of 40 and 60. Women are affected significantly more often than men.
Inclusion body myositis
Inclusion body myositis has been differentiated from polymyositis for some time. This is an inflammatory muscle disease that occurs mainly in men over the age of 50. Inclusion body myositis causes the same symptoms as polymyositis, but it develops more slowly. Unlike polymyositis, it does not affect any other organs, and the muscle pain typical of polymyositis does not occur with one-body myositis.
There are also differences in terms of diagnostics. The muscle enzymes in inclusion body myositis - in contrast to polymyositis - are not increased. Typically, however, fine tissue examinations (biopsy) reveal so-called inclusion bodies on the affected muscles. These are small particles inside cells or cell nuclei that can be seen under a light microscope. They usually consist of faulty proteins.
Despite all the differences, inclusion body myositis is treated in the same way as polymyositis.
Polymyositis: symptoms
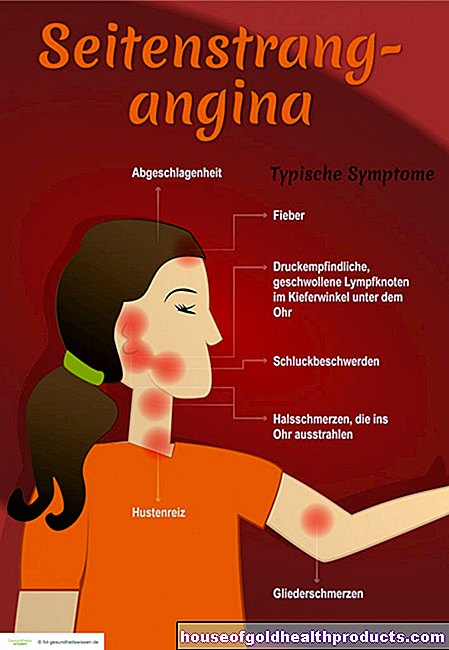
With polymyositis - as with dermatomyositis - unspecific initial symptoms are often found. They include, for example, fatigue and a general feeling of weakness. A fever is also possible. Since such symptoms can also occur in many other diseases (starting with a common cold), they do not initially suggest polymyositis.
On the other hand, it is characterized by symmetrical muscle weakness that progresses over a period of weeks or months, especially in the area of the pelvis, thighs, shoulders and upper arms. Muscle pain also occurs, but less often than in dermatomyositis. Many polymyositis patients also report joint pain.
As with dermatomyositis, involvement of internal organs is also possible with polymyositis. This can lead to swallowing disorders, cardiac arrhythmias, cardiac insufficiency and / or pulmonary fibrosis, for example.
Other possible symptoms are Raynaud's syndrome (blue discoloration of the fingertips) and swollen gums.
In general, polymyositis varies from patient to patient. The main symptom of muscle weakness always occurs. But how severe the symptoms are, how quickly they progress and how severe the disease is overall, is very individual.
Is Polymyositis Curable?
In around 50 percent of those affected, the right treatment leads to complete healing within five years, so that the medication can be discontinued. Often, however, a slight, non-hindering muscle weakness remains in the affected area of the body. In addition, the disease can return.
Treatment can arrest polymyositis in 30 percent of patients. In 20 percent, the therapy does not work - the disease continues.
Risk factors for severe gradients
Polymyositis is often more severe in older patients as well as in male patients. The same applies if the heart or lungs are affected. Concomitant cancer is also a risk factor for a severe course of polymyositis. Life expectancy can be reduced in such cases.
Polymyositis: causes
How exactly a polymyositis develops has not been conclusively clarified. However, it is undisputed that it is an autoimmune disease. This means: The immune system attacks the body's own structures due to a dysregulation - in the case of polymyositis, the muscles.
Dermatomyositis is also an autoimmune disease. If you take a closer look, however, it becomes clear that the autoimmune reaction in polymyositis proceeds differently than in dermatomyositis:
- In dermatomyositis, the antibodies produced by the so-called B lymphocytes are primarily responsible for the muscle damage - and indirectly: They damage small blood vessels in the muscles (and skin) and thus cause the typical symptoms.
- In polymyositis, on the other hand, it is not the blood vessels that are damaged, but the muscle cells themselves. The culprit is also different: special T lymphocytes (T killer cells) of the immune system are active here.
But why does the defense system of polymyositis patients suddenly fight the body's own structures? There is (still) no final answer to this question. However, experts suspect that the misdirected immune reaction is genetic and may be triggered by external influences such as infections.
Polymyositis: diagnosis
Polymyositis is diagnosed using the same diagnostic methods as dermatomyositis:
- Blood tests: As with dermatomyositis, certain blood values are elevated (e.g. muscle enzymes, CRP, blood sedimentation) and auto-antibodies are often detectable (such as ANA).
- Electromyography (EMG): Changes in electrical muscle activity indicate damage to the muscles.
- Imaging: Methods such as ultrasound or magnetic resonance imaging (MRI) confirm the suspicion.
- Muscle biopsy: A sample taken from the affected muscle tissue shows destroyed muscle cells under the microscope. In addition, T lymphocytes become visible, which accumulate between the muscle cells during polymyositis.
Exclusion of other diseases
For a reliable diagnosis it is important to rule out other diseases with similar symptoms (differential diagnosis). Polymyositis can easily be confused with other muscle diseases, especially when the symptoms are weak and the disease progresses slowly.
This includes, for example, muscular dystrophy. This is a group of hereditary muscle diseases that also have muscle weakness as the main symptom and some of them lead to death at a young age.
Polymyositis: treatment
Like dermatomyositis, polymyositis is first treated with glucocorticoids ("cortisone"). They have an anti-inflammatory effect and dampen immune reactions (immunosuppressive effect). Other immunosuppressants are added later, for example azathioprine, cyclosporine or methotrexate.
As with dermatomyositis, experts also recommend regular physiotherapy and targeted muscle training. This helps polymyositis patients to maintain their mobility and prevent muscle wasting.
Tags: teeth news baby toddler