Phenylketonuria
Marian Grosser studied human medicine in Munich. In addition, the doctor, who was interested in many things, dared to make some exciting detours: studying philosophy and art history, working on the radio and, finally, also for a Netdoctor.
More about the experts All content is checked by medical journalists.Phenylketonuria (PKU) is a congenital, hereditary disease of protein metabolism. It prevents the breakdown of the amino acid phenylalanine. This accumulates in the body and disrupts the child's brain development. If left untreated, phenylketonuria leads to severe intellectual disabilities. However, with timely therapy, patients can lead a normal life. Find out everything about phenylketonuria here!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E70
Phenylketonuria: description
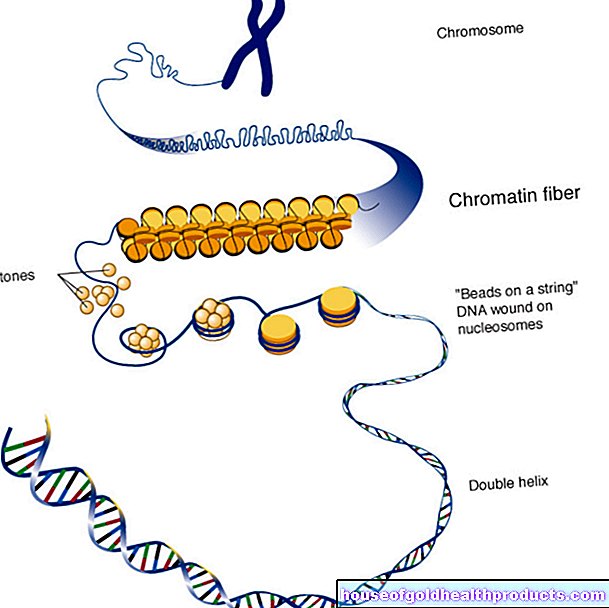
Phenylketonuria (PKU) is an inherited metabolic disease that exists from birth and disrupts the breakdown of the essential amino acid phenylalanine. Amino acids are the basic building blocks of proteins and thus vital metabolic components. Some of them can only get into the body through food, the organism cannot produce them itself. Such amino acids are called essential.
What happens with phenylketonuria?
Amino acids are normally subject to a balance between absorption / construction and breakdown, so that there is always as much available as the body needs. In the case of various amino acids, a deficiency or excess can cause considerable harm and cause various symptoms.
In the so-called classic PKU, the effect of phenylalanine hydroxylase (PAH) is limited or even completely absent. Due to the PAH deficiency, phenylalanine increasingly accumulates in the body. Too high a concentration of phenylalanine disrupts brain development considerably and leads to intellectual disabilities in young patients at an early stage.
Because the normal breakdown of phenylalanine is not possible with the disease, other breakdown products, the so-called phenyl ketones, are formed. They are excreted in the urine and are responsible for the name of the disease.
Atypical phenylketonuria
Even with atypical forms of phenylketonuria, the breakdown of phenylalanine is disturbed. However, the cause is not a defect in the PAH. Instead, the function of a coenzyme, tetrahydrobiopterin (BH4), is restricted. It is indirectly involved in the breakdown of phenylalanine because the PAH needs BH4 to convert phenylalanine to tyrosine.
Because BH4 is also important for the production of the messenger substances dopamine and serotonin, atypical phenylketonuria with BH4 deficiency is usually more complicated than the classic form.
Who does phenylketonuria affect?
PKU is one of the most common congenital metabolic diseases. It is estimated that around one in 7,000 newborns worldwide will develop it, with no difference between girls and boys. Since it is a hereditary disease, several members of a family are often affected.
Phenyketonuria: symptoms
At first, babies with phenylketonuria do not show any symptoms of the disease. The first problems do not appear until the fourth to sixth month of life, if the disease has not yet been recognized and treated. Above all, the disturbed brain maturation causes massive complications over time. Symptoms of untreated PKU include:
- a strong mental deficit. The brain damage progresses through puberty and then stagnates. The affected children are then usually severely mentally handicapped.
- Fits (seizures) (epilepsy). Because of the damage, the nerve cells of the brain are particularly sensitive and overexcitable. Frequent epileptic seizures are the result.
- motor disabilities. Not only the brain cells, but also the muscles of the patient can be over-excited. That is why it often becomes tense (spasticity), which leads to various movement disorders.
- Behavioral disorders. Some children with phenylketonuria are hyperactive and unusually aggressive, and outbursts of anger are also more common.
- a small head (microcephaly). Because the patient's brain does not develop properly, head growth also lags. The small head circumference compared to their peers is particularly noticeable in older children.
- a noticeable smell. PKU produces certain breakdown products of phenylalanine that smell similar to mouse excrement. These substances are mainly excreted in the urine, but also partly through the skin.
- eczema-like skin changes
Because the production of the pigment melanin is also disturbed in phenylketonuria, many sufferers have very light, sun-sensitive skin and white-blonde hair. The iris of the eyes is also light blue to transparent and allows the reddish fundus to shine through.
The PKU symptoms vary in severity from person to person. The main reason for this is that the activity of phenylalanine hydroxylase (PAH) is restricted differently in each patient. Some still have a certain residual activity, so that less phenylalanine accumulates in the organism. Others show no enzyme activity whatsoever - the disease progresses correspondingly faster and more seriously.
Phenylketonuria: causes and risk factors
Phenylketonuria is a hereditary disease. Numerous genetic mutations are now known that lead to a defect in PAH. The type of mutation determines the extent to which the breakdown of phenylalanine is restricted.
PKU is inherited recessively, which means that a person can be a carrier of an altered gene without developing the disease. Likewise, people with phenylketonuria can father healthy children.
Only if both parents have mutations in their genetic makeup is there a certain probability that their offspring will develop phenylketonuria. If the parents are both not only carriers of the genes, but also have PKU themselves, all children together will also develop it.
Phenylketonuria: examinations and diagnosis
Since the serious consequences of phenylketonuria can be prevented by starting treatment in good time, it is particularly important to discover the disease as early as possible. In Germany, children are examined for various congenital diseases, including PKU, as part of a general examination (newborn screening) on the third day after birth.
Tandem mass spectrometry
Many congenital metabolic disorders are now diagnosed with the help of so-called tandem mass spectrometry. It enables the newborn's blood to be examined quickly and easily. In addition to phenylketonuria, doctors can detect more than 20 other diseases within a few minutes.
Guthrie test
The Guthrie test, named after its inventor, also makes it possible to diagnose PKU. To do this, a small amount of blood is taken from the child's heel and applied to a piece of filter paper. In the laboratory you can then determine whether the concentration of phenylalanine is increased.
The Guthrie test was introduced in the 1960s and has long been the standard method for diagnosing phenylketonuria. However, it has disadvantages compared to tandem mass spectrometry. The Guthrie test only delivers a result after five days, which is also prone to errors. For example, factors such as the child's diet or possible antibiotic therapy falsify the results. The Guthrie test is still in use in some countries, but is generally no longer used in Germany.
Other tests
If the newborn screening reveals a suspicion of phenylketonuria, a further examination follows for confirmation. This can also be used to determine the exact concentration of phenylalanine in the blood.
Finally, it is important to distinguish whether it is a typical (classic) or atypical PKU. Special tests are also available for this, such as the tetrahydrobiopterin stress test. The distinction is important because atypical phenylketonuria is treated differently than the classic form.
Amniotic fluid examination
Phenylketonuria can already be diagnosed during pregnancy (prenatal diagnosis). To do this, a small amount of amniotic fluid is taken from the mother's amniotic sac and the cells of the unborn child contained in it are examined. Any genetic defects that cause PKU can be identified in this way.
With newborn screening, however, phenylketonuria is usually discovered early enough to be treated. Because an amniotic fluid test is always associated with a certain risk, its use for diagnosing PKU is usually not useful.
Phenylketonuria: Treatment
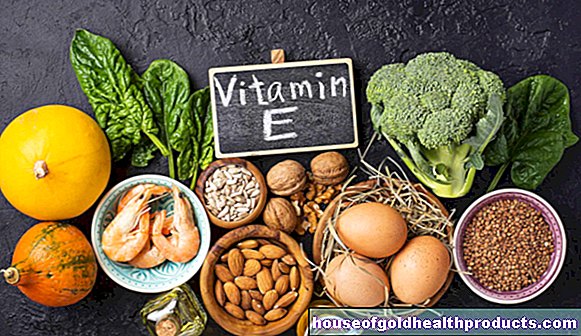
There is only one way to counteract the excess phenylalanine in PKU: The affected children have to follow a special diet in order to take in as little phenylalanine as possible with their food. They also need certain food supplements to replace substances that would be formed from phenylalanine in healthy children.
Therapy must begin before the first symptoms of a developmental disorder appear, i.e. within the first two months of life. Brain damage that has already occurred cannot be reversed.
Nutritional therapy with the PKU diet
All natural proteins consist of about five percent of the amino acid phenylalanine. Most foods contain far more of it than the body needs. This is not a problem for a healthy person because he breaks down and excretes the excess amounts of phenylalanine.
Patients with phenylketonuria, on the other hand, have to do without natural proteins for the most part. Industrially manufactured special products replace the missing food components. On the one hand, one wants to prevent an excess of phenylalanine, on the other hand, the patient should be supplied with substances that they would otherwise lack, such as tyrosine, which is formed from phenylalanine.
However, the goal of the PKU diet is not to completely stop the absorption of phenylalanine. Because the organism needs a certain amount of the amino acid for important metabolic processes. Achieving the right concentration poses a great challenge for doctors and patients and requires a lot of discipline.
The diet must therefore be adhered to for a lifetime, but particularly strictly until the age of six. Because the brain develops very strongly up to this age and is therefore particularly susceptible to damage. In adulthood, high concentrations of phenylalanine do not cause brain damage as they do in children. However, they can be the trigger for other neurological complaints such as poor concentration or slowed reactions.
Diet treatment for phenylketonuria should begin at a specialist metabolic disease center. Because it is not possible in every clinic to instruct parents on the diet. This is best done with the help of diet counseling, which shows how to go about the diet and regularly monitor blood phenylalanine levels.
Treatment of atypical phenylketonuria
In atypical forms of PKU, the missing coenzyme BH4 and certain messenger substances such as dopamine and serotonin are artificially replaced. In some cases, the patient must also be on a low-phenylalanine diet.
Phenylketonuria During Pregnancy
If you are pregnant and have phenylketonuria yourself, you should consider the following:
- Stick to your diet particularly strictly!
- Have your phenylalanine blood count checked at frequent intervals. Because the concentrations of phenylalanine in the unborn child are about twice as high as in the pregnant woman. In addition to the brain, they can also damage the heart and eyes of the unborn child. Malformations of the child's skeleton can also arise from high phenylalanine levels during pregnancy.
- In order to rule out brain damage to the child in early pregnancy, women with phenylketonuria should plan pregnancy carefully and take precautions from the outset.
- In pregnant women with phenylketonuria, a diet that is not strictly adhered to can lead to a miscarriage (spontaneous abortion).
- In any case, pregnant women with phenylketonuria should seek advice and guidance from a doctor.
Phenylketonuria: disease course and prognosis
If phenylketonuria is diagnosed early, if possible in the newborn, and if the special PKU diet is followed, the prognosis is usually good. The children develop spiritually and have an average life expectancy.
If left untreated, however, the brain damage leads to severe mental developmental disorders that cannot be corrected later. Those affected have a normal life expectancy, but their intelligence quotient is almost always very far below the norm.
The rare atypical form of phenylketonuria, in which BH4 deficiency is present, is a special case. This variant of phenylketonuria can lead to progressive neurological damage with severe cramps despite diet.
Tags: sports fitness therapies laboratory values