Strep infection
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.Streptococcal infections are usually harmless and heal completely with antibiotic therapy. In some cases, however, the bacterial infection causes serious problems. Read here which diseases are triggered by streptococci, which symptoms occur and how they are treated!
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. B95

Brief overview
- What is strep infection? Infection with the bacterium Streptococcus, of which there are different types
- Symptoms: Which symptoms occur depends on the particular disease. Symptoms range from a harmless sore throat to life-threatening blood poisoning.
- Treatment: antibiotics (penicillin, alternatively gentamycin, aminoglycosides, macrolides or cephalosporins), analgesic and antipyretic drugs, surgery for necrotizing fasciitis and myositis
- Diagnostics: Typical appearance, course of the disease, smear from the wound or throat, bacterial culture, rapid test
- Causes: Infection with the bacterium Streptococcus
- Risk factors: Very young or very old age, weakened immune system
- Prevention: hygiene measures, pneumococcal vaccination, antibiotics during childbirth to prevent infection of the baby
What are strep?
Streptococci are a large group of spherical bacteria of which there are different types. Most types of streptococci are harmless and are found naturally on the skin and on mucous membranes, in the intestines, in the mouth and throat and in the vagina. Why some people are colonized with streptococci but do not become ill, and why an illness breaks out in others, is not fully understood.
Doctors suspect that the immune system plays a crucial role. Newborns, toddlers and children are likely to get sick because their immune systems are not yet fully developed. Streptococcal infections are most common in adults when their immune systems are weakened. Stress also plays a role here, which has a negative effect on the body's defenses. The immunocompromised, the chronically ill and the elderly are particularly at risk.
After surviving a streptococcal infection, you are not immune, which means that the disease may recur if you get infected again.
Strep infection during pregnancy usually does not cause problems in healthy women. Most pregnant women do not notice the bacterial colonization of their vagina. Complications only arise when the baby becomes infected with the pathogens during birth. In rare cases this can develop into life-threatening blood poisoning (neonatal sepsis).
Classification of streptococci
Streptococci are a large group of bacteria. There are essentially two different ways to classify strep:
Ability to dissolve red blood cells
Some streptococci are able to destroy red blood cells. Doctors speak of hemolysis or hemolytic streptococci. When the red blood cells break down, the red blood pigment hemoglobin is released.
Alpha-hemolytic streptococci: Hemoglobin is only partially broken down. Since this creates greenish degradation products, doctors refer to this type of bacteria as "greening streptococci". They can be found, for example, in the oral cavity (caries bacteria).
Beta hemolytic streptococci: Beta hemolysis means that the streptococci completely break down the red blood pigment. An example of beta-hemolytic streptococci is Streptococcus pyogenes.
Gamma hemolytic streptococci: they are unable to break down red blood cells. These include enterococci, which were previously counted among the streptococci, but are now a separate bacterial species.
Classification according to certain cell wall components (Lancefield classification)
On the basis of certain cell wall components, doctors differentiate between streptococci of groups A to Q. For humans, group A (Streptococcus pyogenes) and group B (Streptococcus agalactiae) are predominantly pathogenic. Streptococci from other groups, such as those from group C (Streptococcus equi, Streptococcus dysgalactiae) attack livestock such as horses or cattle.
Which diseases are caused by streptococci?
Streptococci cause a variety of different diseases. Examples of the most common diseases are:
A streptococci (main representatives Streptococcus pyogenes):
- Tonsillitis (tonsillitis, angina tonsillaris)
- Otitis media
- sinus infection
- Sore throat (pharyngitis)
- Scarlet fever
- Contagious ringworm (impetigo contagiosa)
- Rotlauf (Erysipelas)
- Necrotizing fasciitis
- Myositis
- Inflammation of the glans on the penis (balanitis)
- Blood poisoning (sepsis)
- Toxic shock syndrome
B streptococci (main representatives Streptococcus agalactiae):
- Neonatal sepsis
- Wound infections
- Cystitis
- Meningitis
Pneumococci (Streptococcus pneumoniae):
- Inflammation of the lungs (pneumonia)
- Meningitis
- Blood poisoning (sepsis)
- Overwhelming post-splenectomy infection (OPSI)
Oral streptococci (Streptococcus viridans, greening streptococci):
- Dental caries (streptococcus mutans)
- Appendicitis
- Inflammation of the lining of the heart (endocarditis)
How are streptococci transmitted?
Streptococci enter the body in different ways:
Droplet infection: The pathogen is transmitted via coughing, sneezing or kissing and thus reaches the mucous membranes in the throat. The streptococci multiply there and - depending on the type of pathogen - trigger diseases such as throat or tonsillitis.
Smear infection: With a smear infection, the pathogen enters the body through direct contact with an infected person or a contaminated object. It is possible that the streptococci penetrate the skin or the mucous membrane through the smallest injuries and multiply there. Examples of diseases are ringworm, rot and necrotizing fasciitis.
During childbirth: If the pregnant woman's vagina is colonized with group B streptococci, it is possible that the child could become infected during childbirth.
Streptococci are also sexually transmitted!
Are Streptococci Contagious?
If left untreated, patients with acute strep infections are contagious for up to three weeks. If there are purulent infections of the skin, even longer. If those affected receive effective antibiotic therapy, the risk of infection disappears after 24 hours.
What are the symptoms of a strep infection?
The symptoms or signs of a streptococcal infection depend on the type of pathogen. The symptoms usually develop around two to four days after infection (incubation period).
Group A streptococci (Streptococcus pyogenes):
Streptococcus pyogenes bacteria are common pathogens causing typical infectious diseases such as tonsillitis and scarlet fever. They occur localized (affecting certain areas of the body) or systemic (affecting the whole body).
Symptoms of inflammation of the throat (pharyngitis) or tonsillitis (angina tonsillaris)
- Mostly children between the ages of six and twelve are affected.
- Sore throat, difficulty swallowing
- fever
- Typically, there are usually no other cold symptoms such as coughing or runny nose (these are usually caused by viruses).
- Small children may refuse to eat and may also suffer from nausea, abdominal pain and vomiting.
Symptoms of scarlet fever
Scarlet fever develops from strep throat inflammation. After about twelve to 48 hours, the typical crimson rash forms on the folds of the armpits and groin. It eventually spreads over the entire body, the area around the mouth characteristically remaining pale. In addition, there are purulent coatings on the lining of the throat and palate, and the lymph nodes on the neck are swollen. From the third day of illness the tongue is very red (raspberry tongue). After about seven days, the skin begins to peel off.
Symptoms of skin and soft tissue infection
Ringworm (impetigo contagiosa): Typical symptoms are superficial skin infections, purulent blisters on the mouth and nose or on the legs, which later become encrusted. Typically, there is no fever, and those affected hardly feel sick. A painful red rash around the buttocks (perianal dermatitis) occurs in toddlerhood. Affected children often avoid bowel movements, which in some cases develops into constipation.
Erysipelas: The erysipelas usually occurs in older adults. The pathogen infects the skin, subcutaneous tissue and local lymphatic vessels. The skin is very red and painful. In addition, there is a high fever.
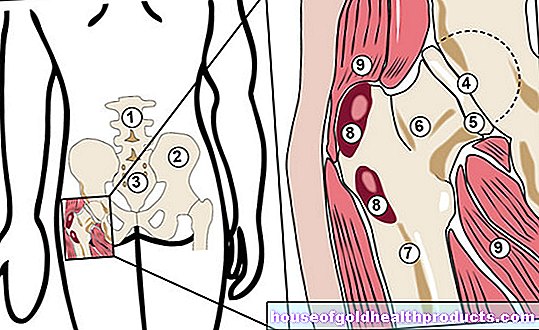
Necrotizing fasciitis: In necrotizing fasciitis, the streptococci affect muscles and muscle fascia (muscle sheaths). The affected areas become red, hot, swollen, and blister. Within a few hours or days, the skin turns bluish-red. Affected people feel sick, have pain, fever and chills. In some cases, complete death (necrosis) of the skin, subcutaneous tissue and muscle fascia occurs later. Seldom blood poisoning or toxic shock syndrome develop from necrotizing fasciitis.
Primary myositis: In the very rare primary myositis, the muscle tissue is infected and changes to the skin are not visible. Those affected suffer from severe pain and have a high fever and chills, and the risk of blood poisoning or TSS is significantly increased.
Toxic shock syndrome (TSS): If the streptococci are washed into the blood, blood poisoning develops. If left untreated, circulatory failure quickly occurs, followed by multiple organ failure.
Group B streptococci:
Symptoms of neonatal sepsis
The vagina of around ten to 35 percent of all pregnant women is infected with B streptococci, but only around one percent of women actually show symptoms (discharge). About half of all children of women who are carriers are infected with the pathogen during birth.Of these, 0.5 to 1 percent develop newborn sepsis.
Infants with neonatal sepsis develop a high fever and may develop pneumonia and / or meningitis.
Obstetricians and gynecologists recommend a smear test between the 35th and 37th week of pregnancy to determine whether the pregnant woman is infected with streptococci. With antibiotics during childbirth, the risk of transmission can be minimized to a large extent!
Symptoms of Pneumococcal Infection
The symptoms of pneumococcal infection depend on the condition that is causing them. The pneumococci are transmitted by coughing or sneezing and colonize the mucous membranes in the nasopharynx. Pneumococci are found in the airways in almost half of the healthy population. However, they are kept in check by an intact immune system and thus go unnoticed.
If the immune system is weakened, the pathogens multiply uncontrollably, spread and can trigger a severe form of pneumonia. Infants and young children, but also the elderly, are particularly at risk. A pneumococcal infection can lead to serious, sometimes life-threatening complications such as meningitis, blood poisoning (sepsis), inflammation of the joints (arthritis) or inflammation of the lining of the heart (endocarditis).
How is strep infection treated?
Harmless streptococcal infections are usually treated on an outpatient basis; in more severe cases, treatment is given in hospital.
Medication
The treatment of choice for strep throat is penicillin - an antibiotic. A bacterial infection cannot be brought under control without antibiotics or with “natural healing methods”. Depending on the severity of the disease, the patient receives the antibiotic in the form of tablets or as an infusion. If the patient does not respond adequately to the penicillin - for example because they are resistant to the active ingredient - the doctor may prescribe a different antibiotic. The same applies if the patient is allergic to penicillin. Combinations with other antibiotics such as gentamycin, aminoglycosides, macrolides or cephalosporins may be used.
If there is fever or pain at the same time, the doctor treats the patient with antipyretic and pain reliever medication.
surgery
In the case of constantly recurring streptococcal infections (angina tonsillaris, tonsillitis) it makes sense under certain circumstances to remove the tonsils.
In some cases, when infected tissue has died (necrotizing fasciitis) or is badly damaged (myositis), it may be necessary to surgically remove it.
Treatment of pregnant women who tested positive
If the pregnant woman is found to be infected with the bacterium as part of the streptococcal screening at the end of the pregnancy, she will also receive penicillin from the start of labor or after the amniotic sac has ruptured. The actual aim of treatment is not to treat the mother, but to protect the baby from being infected during birth.
Investigation and diagnosis
Usually, doctors diagnose strep infection based on how it looks and how the disease has progressed. For example, scarlet fever shows a typical rash. In pregnant women who are colonized with streptococci but show no symptoms, the doctor determines the colonization by means of a preventive streptococcal test. The cost of the test is around 25 to 40 euros. As a rule, they are not covered by the health insurance companies.
If a strep infection is suspected, the doctor will take a swab from the suspicious location. This is, for example, the throat, a skin wound or the vaginal mucous membrane. To do this, he takes a sample from the skin or mucous membrane using a sterile cotton swab and then creates a bacterial culture. For this purpose, the bacteria are multiplied on a special substrate. Depending on whether and in what form they grow or how they look under the microscope, the doctor will clearly identify them.
There are rapid tests for some types of streptococci (such as a sore throat); the results are available after just a few minutes. They are used when there is doubt as to whether the infection is viral or bacterial.
There is a second rapid test to identify pneumococci. For this, the doctor needs a fresh urine sample in which the streptococci can be detected.
Course of the disease and prognosis
course
Streptococcal infections can usually be treated well with antibiotics. If left untreated, there is a risk of serious long-term effects after a few weeks, especially in the case of infections with group A streptococci (Streptococcus pyogenes). These include acute rheumatic fever with inflammation of the heart valves and the heart muscle. If the kidney is affected, the kidney corpuscles are often damaged (glomerulonephritis).
The reason for this is not the bacteria themselves, but the defense bodies (antibodies) that the immune system has formed against the pathogens. They resemble certain cells from muscles, connective tissue and the kidney. The antibodies are therefore not only directed against the streptococci, but also falsely against harmless, endogenous tissue. Doctors speak of an "autoimmune reaction".
Most newborns who recover from sepsis usually have no long-term effects to fear. However, newborns who survive meningitis (meningitis) may have developmental delays, brain damage, seizures, or hearing loss.
forecast
In the case of harmless streptococcal infections such as tonsillitis or scarlet fever, the prognosis is very good - treatment with antibiotics usually leads to a complete cure.
The prognosis is less favorable for more serious diseases such as necrotizing fasciitis. If therapy is started late, around 30 percent of patients die, and up to 85 percent for toxic shock syndrome.
Causes and Risk Factors
Streptococcal infections are caused by an infection with the bacterium Streptococcus. Depending on what kind of pathogen it is, streptococci cause different diseases. Types of streptococci that most commonly cause disease are:
- Streptococcus A (Streptococcus pneumoniae)
- B streptococci (Streptococcus agalactiae)
- Pneumococci (Streptococcus pneumoniae)
- Oral streptococci (Streptococcus viridans)
Prevent
Hygiene measures
Infection with pneumococci is possible in different ways. The options for protecting yourself against transmission are correspondingly diverse. Smear infections - i.e. transmission through direct contact - can be prevented through hygiene measures. Wash your hands several times a day, especially after coming into contact with infected people. Against a transmission by droplet infection - for example via coughing or sneezing - help, as well as with viral pathogens (e.g. coronavirus), distance and etiquette (e.g. coughing and sneezing into the crook of the elbow).
vaccination
Pneumococcal vaccination protects against infection with Streptococcus pneumoniae. The risk of developing pneumonia is age-dependent. Children in the first two years of life and the elderly are particularly at risk. The same applies to people who suffer from chronic lung diseases, diabetes mellitus or neurological diseases. Also at risk are immunocompromised, chronically ill or patients with a cochlear implant (a hearing prosthesis) or a liquor fistula (an artificial connection between the body surface and the cerebral ventricles filled with cerebrospinal fluid, usually resulting from a fracture of the base of the skull).
The Standing Vaccination Commission (STIKO) therefore recommends pneumococcal vaccination for all babies from the age of two months, for all people from 60 years and for people with the diseases mentioned above.
Protection against transmission at birth
Colonization of the mother with streptococci during pregnancy does not initially pose a threat to either the mother or the child. Health problems only arise if the baby is infected with the pathogen during birth. To prevent transmission, pregnant women who have found streptococci in a test during pregnancy (smear) are given an antibiotic at the start of labor or immediately after the rupture of the bladder, in accordance with current guidelines.
A caesarean section is only an alternative if it is performed before labor begins and the amniotic sac ruptures. If the amniotic sac has already cracked, the operation does not offer any protection against infection of the child. In this case, too, the mother is given antibiotics.
Tags: drugs news healthy workplace