Knee pain
and Martina Feichter, medical editor and biologistJens Richter is editor-in-chief at Since July 2020, the doctor and journalist has also been responsible as COO for business operations and the strategic development of
More posts by Jens Richter
Martina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Knee pain can have very different characters. Sometimes they arise suddenly and in a recognizable connection with an exposure, a fall or an accident. Then there are often other symptoms such as swelling and bruising. Knee pain can also be caused by chronic joint wear or various diseases. Read here what can be behind knee pain and how it can be alleviated.

Brief overview
- Description: Knee pain can occur suddenly or gradually, only at rest or when moving or exercising. Sometimes they are limited to a specific area (inside, outside, or front of the knee joint, hollow of the knee). The knee pain is often accompanied by other complaints (redness, swelling and overheating of the knee joint, bruises, etc.).
- Possible causes: injuries (contusion, strain, cruciate ligament tear, meniscus tear, kneecap dislocation, kneecap fracture, etc.), inflammation (bursitis, rheumatoid arthritis, rheumatic fever, ankylosing spondylitis, gout, reactive arthritis (Reiter's disease), systemic lupus erythematosus, etc.) of the knee joint (gonarthrosis), parapatellar pain syndrome, Baker's cyst, etc.
- Examinations: doctor-patient discussion (anamnesis), physical examination, possibly imaging procedures (x-ray, ultrasound, magnetic resonance imaging, computed tomography, scintigraphy) and further examinations (arthroscopy, blood tests, angiography, tissue samples, etc.)
- Treatment: depending on the cause. For example, rest, immobilization, application of cold or heat, pain relievers, ultrasound therapy, electrical stimulation therapy, surgical treatment of open wounds, treatment of underlying diseases (rheumatism, psoriatic arthritis, etc.) are possible.
Knee pain: symptoms & localization
Knee problems can appear suddenly (e.g. in the case of injuries) or gradually increase. The latter is the case with increasing wear and tear of the knee joint (knee arthrosis = gonarthritis). Sometimes the knee pain is so severe that walking, standing or even sitting for a long time is hardly possible. Depending on the cause, knee pain is only a temporary (treatable) health problem or a daily companion that one has to learn to live with.
When the pain occurs is also very variable and can indicate the possible cause:
- Pain at the start (pain at the start): This is the name given to knee pain that is noticeable at the beginning of a movement in the joint and subsides with further movement. The cause is often wear and tear (osteoarthritis) of the knee joint (osteoarthritis of the knee).
- Movement pain: If the knee hurts more or less continuously during movements, this is often due to a recent injury (of tendons, ligaments, bursae, menisci etc.).
- Exercise pain: If knee pain only occurs when the joint is loaded, this can indicate, for example, a meniscus injury. Sometimes the knees hurt especially when they are put under strain when climbing stairs. The possible cause is a certain form of bursitis (pes anserina bursitis).
- Rest pain: If the knee pain occurs (also) at rest, the reason could be rheumatoid arthritis.
The localization of knee pain can - depending on the cause - also be very different:
- For example, knee pain on the inside of the joint can be due to damage to the medial meniscus. Pain in the inside of the knee (or slightly below) also occurs with bursitis of the pes anserina bursitis type.
- Knee pain on the outside can be caused by damage to the external meniscus. But there are other possible causes as well. For example, a so-called "runner's knee" may be present: it is a painful irritation of the fiber tension that pulls from the outside of the thigh to the shin. Passionate runners are particularly affected.
- Front knee pain is often grouped under the term patellofemoral pain syndrome or femoropatellar pain syndrome. The triggers can be very different (incorrect and overloading, injury or malformation of the kneecap, injury or inflammation of the bursa in the front knee area, etc.).
- A Baker's cyst, among other things, can be responsible for pain in the hollow of the knee. This is a fluid-filled cavity in the hollow of the knee.
Depending on the cause, the knee pain is often accompanied by other complaints (accompanying symptoms). For example, inflammation-related pain in the knee can be accompanied by swelling, redness and overheating in the joint area. If the knee pain is associated with increasingly restricted mobility of the knee joint, the cause is usually progressive wear and tear of the joint (knee osteoarthritis). The complaints often increase in cold and wet weather ("weather sensitivity").
Knee pain: most common causes
Knee pain can have many different causes. In addition to injuries, this also includes overstressing and improper strain on the joint. However, pain can also arise if a knee joint is not used too often and the associated muscles are untrained. In addition, knee pain can be caused by wear and tear, metabolic disorders, autoimmune diseases, and infections.
Injuries as a cause of knee pain
An injury to the cartilage, ligaments, or menisci is often the cause of knee pain. Such injuries do not only occur in sport or in hard physical work. You can also injure your knee in everyday life. The combination of bending and twisting as well as sudden stopping movements with increased shear forces are particularly risky for the knee joint. Here is an overview of the most important injuries:
- Bruises are a common cause of knee pain. A bruise usually occurs outside the joint capsule as a result of a shock, blow or fall. The skin in the affected area turns bluish-red in color.
- Strains are overstretching muscles, ligaments, the capsule or the tendons around the joint. You will notice a bruise and pain. In addition, the affected knee feels less stable to the patient for a while.
- Muscle and tendon tears in the knee joint usually only develop in otherwise healthy people when the force is applied to a great extent - and therefore particularly often in athletes. Collateral ligament, tendon attachment or patellar tendon tears are usually associated with a bruise and severe functional impairment and loss of stability.
- Meniscal tears are often caused by a combination of flexion and rotation in the knee joint. The meniscus can partially or completely tear off the roof of the tibia. The patients develop the typical "meniscus pain" and an often bloody joint effusion. If part of the meniscus moves into the joint space due to injury, the knee joint will no longer function properly. It can even be completely blocked. Torn injuries particularly often affect the meniscus on the inside of the joint (inner meniscus).
- Strong shear forces in the knee joint can tear the cruciate ligament. Stopping movements, changes of direction or external violence (like in football) are particularly dangerous. If these movements and forces cannot be absorbed by the surrounding muscles because they are too sudden or too strong, a cruciate ligament can tear. The anterior cruciate ligament is most commonly affected.
- A kneecap dislocation (patellar dislocation) is when the kneecap jumps out of its guide to the side. This can lead to severe pain in the knee, bruises, tears in the ligamentous apparatus of the kneecap and damage to the cartilage.
- Broken bones can also be the cause of knee pain. The injury can affect the head of the shinbone, the so-called joint rollers (condyles) of the thighbone, or the kneecap. Bone injury can also occur with a cruciate ligament tear if a piece of the bony anchorage is torn out.
- Open wounds such as abrasions or cuts are common and mostly harmless injuries to the knees. If the injuries are deeper, there is an increased risk of infection. If the doctor suspects an injury to the joint capsule in a patient and thus an opening of the joint interior, an operation must be performed immediately.
Inflammation as a cause of knee pain
Sometimes knee pain is caused by a non-bacterial inflammatory disease of the joint. These include rheumatic diseases and certain metabolic disorders that attack the inside of the knee joint:
- In chronic, mostly intermittent rheumatoid arthritis (chronic polyarthritis), immune cells attack the synovial membrane. This becomes inflamed and produces inflammatory substances that destroy the connective tissue and the articular cartilage.
- Bechterew's disease (ankylosing spondylitis) is one of the rheumatoid diseases. In addition to inflammation, there is an increasing curvature of the spine. Patients usually try to compensate for this curvature by flexing their hips and knees. Knee pain is one of the possible consequences.
- Arthrosis is the term used to describe the wear and tear of the joints. The cartilage coating on the joints gradually wears off until the bones rub against each other without protection.
- In gout, the level of uric acid in the blood is greatly increased. The excess uric acid is then deposited in the joints (such as the knee joint) in salt crystals, irritating and damaging the synovial membrane and cartilage. Gout manifests itself in the knee in stages with very painful swelling and overheating.
- In pseudogout (chondrocalcinosis) calcium salt crystals form, which are deposited in the cartilage. This often has similar consequences as the deposition of uric acid crystals in gout.
- Reactive arthritis (previously: Reiter's disease or Reiter's syndrome) is another representative of the rheumatoid group. It is an inflammation that can occur after certain bacterial infections of the intestine, urinary tract or genital organs. It can cause knee pain, among other symptoms.
- Rheumatic fever is caused by certain bacteria, a type of streptococcus. It can affect the knee and other joints, as well as the heart, kidneys and nervous system.
- Systemic lupus erythematosus is an autoimmune disease, i.e. a disease in which the immune system attacks the body's own cells. So-called immune complexes are formed from antibodies and the attacked cell structures. They can be deposited in the knee, among other things, which can lead to painful inflammation of the synovial membrane.
- Psoriatic arthritis also belongs to the rheumatoid group. It is a chronic inflammation of the joints that occurs in connection with psoriasis. If the knee joint is affected, the resulting knee pain will progressively worsen. But there are also longer symptom-free phases.
Other causes of knee pain
- The so-called parapatellar pain syndrome (chondropathia patellae) is quite common. Those affected feel pain in the kneecap area. The reasons for this are often unclear. Sometimes this is due to a misalignment of the kneecap or an inflammation of the tendons or bursa.
- Tendon and bursitis can be triggered by injuries, infections or overuse.
- The runner's knee (ilio-tibial ligament syndrome or tractus syndrome) is often the reason for stress-related knee pain on the outside of the joint, especially in runners. The symptoms are caused by irritation of the broad, tight fiber cord that runs on the outside of the thigh and attaches to the shin (iliotibial tract). The irritation is due to repeated incorrect or excessive strain on the knee.
- A fold of the mucous membrane on the back of the kneecap (plica mediopatellaris) constantly slides over the articular cartilage when the joint moves. Over time, this can lead to cartilage damage and pain in the knee.
- A softening of the cartilage behind the kneecap (Chondromalacia patellae), an early form of cartilage wear, can also cause knee problems.
- Osteochondroses are disorders of bone formation in children. They occur during the growth phase and are noticeable, among other things, by knee pain.
- Osteonecrosis is the death of a section of bone. The cause can be a septic (caused by bacteria) or aseptic nutritional disorder of the bone. Examples of aseptic osteonecrosis are Osgood-Schlatter's disease and Ahlbaeck's disease. Injuries can also lead to osteonecrosis if bone nutrition is interrupted.
- The term Baker's cyst refers to protuberances in the posterior joint capsule that penetrates between the muscles of the hollow of the knee. A Baker's cyst usually manifests itself as a soft swelling in the back knee and pain in the hollow of the knee.
- Dysfunction in the hip joint can lead to knee pain. Either the pain actually originates in the hip and only radiates to the knee. Or the disruption of the hip function impairs the chain of motion and causes improper stress on the knee. This can cause knee pain over time.
- Hemophilia is a hereditary disease in which blood clotting is impaired. Among other things, this can lead to sudden joint bleeding.
- Malignant as well as benign tumors can also be the cause of knee pain. They can occur in bones, fat or connective tissue, in blood vessels or in the inner lining of the joint.
- Occasionally, there is a psychosomatic cause behind chronic knee pain.
Risky sports
Knee pain is often caused by injuries in sports. Sports with abrupt stopping movements and changes of direction are particularly risky, but also those in which the knee is bent and rotated under heavy load. These include, for example, football, handball, hockey and alpine skiing. But weight training also often leads to painful bruises, ligament strains and damage to the meniscus or cruciate ligament.
Swimming can also cause knee pain. The so-called swimmer's knee, for example, when breaststroke is created by repeated rotational movements in the knee joint. Fins increase the stress on the knee and ankle joints. Turning in the pool (roll turning) with competitive swimmers also puts strain on the knees and can cause knee pain.
Knee pain: when do you need to see a doctor?
Obvious reasons for knee pain such as superficial abrasions, slight bruises or strains of the knee joint can usually be treated as a patient yourself and without medical help. In the case of deeper wounds, however, a doctor's visit is urgently necessary. This is especially true if the joint capsule may have been injured. Then there is a risk that germs will have unhindered access to the interior of the joint. If such infections and serious joint injuries are not treated, the joint function can be partially or completely lost - in other words, the joint can stiffen.
See a doctor even if the menisci, ligaments, or cartilage in the knee may have been damaged.
A doctor should also clarify knee pain in the following cases:
- The knee pain is very severe.
- The cause of the pain is unclear.
- The knee pain lasts for several days (despite rest, heat or cold treatment, pain relievers, home remedies, etc.) or progresses in phases.
- The knee pain is accompanied by other symptoms such as reddening, swelling and overheating of the joint, bruising, restricted mobility of the joint or fever.
Knee pain: examinations
When a doctor wants to get to the bottom of the cause of knee pain, they will first seek important information from the patient. In this conversation to collect the medical history (anamnesis), the doctor asks, among other things, since when the pain has existed and whether there is a probable trigger (such as an accident, sporting stress). The exact location of the knee pain (inside, outside, etc.), its course and any underlying diseases (such as rheumatic diseases or metabolic disorders) are also important for the diagnosis.
The doctor will also inquire whether the patient has already attempted therapy (bandage, cooling, pain relievers, etc.) and how well they have worked.
Physical examination
During the physical examination, the doctor tests how far the affected person can bend the knee joint on their own (active flexion) and how far it can be bent painlessly with help (passive flexion). He feels the tendons and ligaments in the knee area for any abnormalities (palpable injuries, tenderness, etc.). An important function test for the cruciate ligaments is the drawer test: If the head of the tibia can be pulled forward in relation to the thigh bone, the anterior cruciate ligament is unstable (torn). If the head of the tibia can be pushed back in relation to the thigh, the posterior cruciate ligament is damaged.
The doctor may also ask the patient to take a few steps up and down to assess the gait pattern. For example, movement restrictions and relieving postures become visible.
Imaging examinations
Imaging examinations are often necessary to clarify knee pain:
- For example, major damage to tendons and ligaments or a knee joint effusion can be detected by means of an ultrasound examination.
- The doctor can use an X-ray examination to discover broken bones or deviations in the position of the joints, as well as assess the thickness of the articular cartilage. Certain bone deformations typical of osteoarthritis or inflammatory joint diseases are also visible on the X-ray.
- In computed tomography (CT), detailed slice images of the knee joint are created using an X-ray beam circling around the patient. Many changes inside the joint can be seen in this way.
- Another tomography method, magnetic resonance imaging (MRI), is particularly well suited for detecting hidden damage to ligaments, tendons or menisci inside the knee joint. The examination does not use X-rays, but rather strong magnetic fields.
- A scintigraphy is a nuclear medicine examination. With the help of radioactively marked substances, the metabolic activity of different tissues is made visible. This can often reveal inflammation, but also dead bone tissue.
Further investigations
The doctor may order further examinations:
- Sometimes an arthroscopy is necessary in order to accurately assess damage to the knee joint. The doctor inserts a flexible instrument equipped with a small camera (endoscope) into the joint through a small incision in the skin. Small knives or pliers can be pushed through parallel working channels, with which damaged cartilage or an injured meniscus can be smoothed, sewn, glued or removed. Even larger operations on the knee joint can now be performed using an endoscope.
- An angiography is an X-ray examination of the blood vessels. The patient is injected with a contrast agent that makes the vessels clearly visible on the X-ray. Circulatory disorders or dead bone parts (osteonecrosis) can be proven to be the cause of knee pain.
- A blood test can indicate infections, autoimmune or rheumatic diseases. Metabolic diseases such as gout can also be detected using blood values.
- Urine or stool tests are particularly carried out to detect germs (such as bacteria), as some pathogens can lead to an inflammatory reaction within the joint.
- In some cases, an examination of the synovial fluid is useful. It is checked whether the liquid has a pathologically altered composition or whether it contains bacteria or antibodies.
- A throat swab is taken if a rheumatic fever is suspected and analyzed in the laboratory.
- Skin examinations indicate possible psoriatic arthritis.
- If a benign or malignant tumor is suspected, a tissue removal (biopsy) may be required.
Knee pain: you can do it yourself
In the case of acute injuries to the knee joint, the first thing to do is to relieve the joint, relieve pain and counteract swelling. Orientate yourself to the so-called PECH rule: break, ice, compression, elevation. The cold causes the blood vessels to contract and a bruise to stop growing. Elevation also reduces blood flow to the injured area. You can also stabilize the knee with a tight bandage (compression).
If the knee pain is caused by irritation or inflammation of the tissue or a bruise, sports ointments and the use of enzyme tablets can help. An enzyme from the pineapple fruit, for example, has an anti-inflammatory and decongestant effect. Quark compresses have also often proven to be anti-inflammatory and analgesic (because they are cooling). If the knee pain is related to a rheumatic disease, however, warmth can be perceived as more pleasant than cold.
If necessary, you can also use pain relievers for knee pain. In the pharmacy you can get over-the-counter preparations from the group of non-steroidal anti-inflammatory drugs (NSAIDs) such as acetylsalicylic acid (ASA), ibuprofen, naproxen or diclofenac. They have an analgesic and anti-inflammatory effect. Consult a doctor or pharmacist for advice on the choice of pain reliever, dosage, and use.
Knee protection for prevention
Suitable footwear, special knee pads and possibly knee braces (the latter are advisable for sensitive people who, for example, have often had knee problems) offer a certain level of protection against injuries to the knee. However, you should only use these if they are absolutely necessary - for example during training, games or competitions.
Regular and balanced training of the entire musculature around the knee joint is more important for the prevention of knee injuries. Strong muscles stabilize the knee joint and can often prevent knee pain.
Knee pain: treatment by the doctor
Effective pain management is very important in managing knee pain. The doctor will recommend or prescribe a suitable pain reliever for the patient. In doing so, he takes into account any contraindications - that is, circumstances that speak against the use of a certain drug. For example, people with a stomach ulcer should not take NSAID painkillers (such as ASA or ibuprofen).
Further treatment for knee pain depends on the cause. If the pain is related to an open injury, for example, this is surgically cleaned and, if necessary, closed. Because of the high risk of infection for the knee joint, special care is important.
A puncture can provide relief in the event of effusions of blood or irritation in the knee. The accumulated liquid is drawn off with a hollow needle.
With some injuries, the pain in the knee can be relieved with bandages or special splints. At the same time, the range of motion of the joint is limited. This allows the damaged structures to heal in peace.
The doctor can also prescribe physical and physiotherapy treatments for knee pain, depending on the cause. These include ultrasound or electrical stimulation therapy, medical baths, manual therapeutic grips and physiotherapy exercises.
If other diseases are the cause of knee pain (rheumatism, psoriatic arthritis, etc.), these must be treated separately.
Knee pain: this is how it develops
Basically, knee pain is a warning sign that should be taken seriously: The pain often signals that the knee should not be stressed. In the case of wear-related knee pain, however, the opposite often applies: Excessive protection of the painful joint can even damage the knee.

Incidentally, not all damage to the knee manifests itself as classic joint pain. For example, pain in the hollow of the knee can be an indication of damage to the knee joint or its connective tissue capsule.
Sometimes pain radiating from the knee is felt elsewhere (such as the surrounding muscles). Conversely, alleged knee pain can have its cause elsewhere: For example, damage and injuries in the hip joint or spine can radiate downwards and express themselves as knee pain.
It is therefore very important to understand the basic structure and function of the knee and to find out the cause even in the case of unclear knee pain.
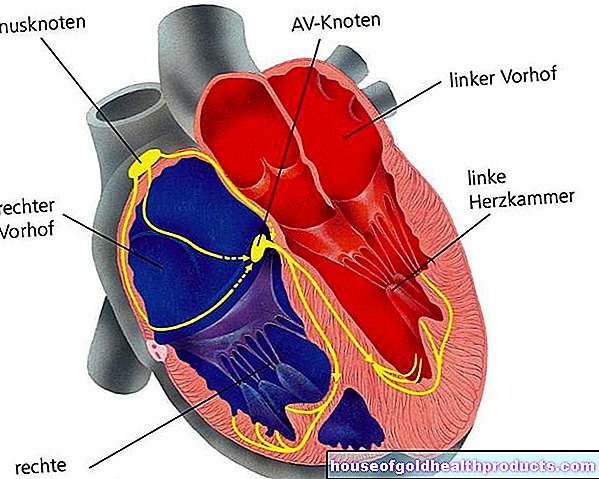
This is how the knee is constructed
Along with the hip and shoulder joints, the knee is one of the most complex and largest joints in the body. Mechanically it works like a one-sided limited hinge. Due to its ingenious internal structure, however, it also offers a certain amount of leeway for slight twists around the longitudinal axis.
Strictly speaking, the knee consists of two individual joints:
- the large, supporting joint between the thighbone (femur) and shinbone (tibia)
- the joint between the kneecap (patella) and the thighbone, which is crucial for the deflection of forces.
Ligaments and tendons give the knee joint support and guidance. The so-called cruciate ligaments (one anterior and one posterior) and lateral ligaments on the outside and inside connect the upper and lower leg bones tightly with one another.
The joint is closed off from the outside by a cover made of connective tissue (connective tissue capsule). Doctors therefore differentiate between damage or injuries inside (intra-articular) and outside the joint (extra-articular).
Muscles and ligaments ensure stability
Muscle power acts on the joint in the front via the strong patellar tendon and the kneecap. Smaller tendons from the back of the thigh muscles attach to the shinbone behind the knee. Smaller muscles work in the opposite direction: They pull from the posterior tibia to the femur. All muscles and ligaments together serve both the movement and the stability of the knee joint.
Menisci and bursa
Inside the knee, two sickle-shaped cartilage discs, the so-called menisci, sit on the shin bone. As a buffer, they absorb shock and pressure loads in the knee and distribute them evenly in the joint. In addition, they ensure that nutrient-rich joint fluid (synovial fluid) is evenly distributed over the joint cartilage.
There are also bursae in the knee. These fluid-filled connective tissue cushions are used as cushions in places where there is particularly high pressure and friction.
Both menisci and bursa are common causes of knee pain in the presence of inflammation or injury.
Tags: Menstruation foot care drugs










.jpg)