Colon cancer
and Martina Feichter, medical editor and biologistFlorian Tiefenböck studied human medicine at the LMU Munich. In March 2014, he joined as a student and has supported the editorial team with medical articles ever since. After receiving his medical license and practical work in internal medicine at the University Hospital Augsburg, he has been a permanent member of the team since December 2019 and, among other things, ensures the medical quality of the tools.
More posts by Florian TiefenböckMartina Feichter studied biology with an elective subject pharmacy in Innsbruck and also immersed herself in the world of medicinal plants. From there it was not far to other medical topics that still captivate her to this day. She trained as a journalist at the Axel Springer Academy in Hamburg and has been working for since 2007 - first as an editor and since 2012 as a freelance writer.
More about the experts All content is checked by medical journalists.
Colon cancer (colorectal carcinoma) is a malignant tumor of the large or rectum. It usually arises from benign intestinal polyps. There is a chance of recovery through an operation. Other methods such as chemotherapy or radiation therapy often support the treatment. Read everything you need to know about the topic: How do you recognize colon cancer? What are its causes and risk factors? How is colon cancer treated? What are the chances of recovery?
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. C17C21C19C18C26C20
Brief overview
- What is colon cancer? Malignant tumors in the large intestine (colon carcinoma) or rectum (rectal carcinoma) are grouped together under the term colorectal carcinoma
- Frequency: In Germany the second most common type of cancer in women and the third most common type of cancer in men
- Symptoms: Colon cancer develops slowly, usually for a long time without symptoms; Possible signs are changed bowel habits, blood in the stool, unwanted weight loss, anemia, possibly abdominal pain, low fever, tiredness, poor performance
- Causes: poor diet (little fiber, a lot of meat and fat), lack of exercise, obesity, alcohol, nicotine, genetic factors, inflammatory bowel disease, type 2 diabetes mellitus
- Treatment: Depending on factors such as location, size and extent; Surgery possible; supportive chemotherapy and immunotherapy
- Prognosis: The earlier discovered and treated, the better the chances of recovery; Daughter tumors (metastases) worsen the prognosis.
Colon cancer: symptoms
Colon cancer usually goes unnoticed for a long time. Symptoms only arise when the tumor has reached a certain size.
If the tumor has already spread to other organs in an advanced stage (metastases), further symptoms may appear.
In the following text you will learn how to recognize colon cancer. But be careful: the symptoms mentioned are not clear signs of colon cancer, but can also have other causes. But you should always have it checked out by a doctor.
Changed bowel movements
Several patients alternately suffer from constipation and diarrhea because the tumor narrows the intestine: the stool initially builds up in front of the tumor. Then it is liquefied by bacterial decomposition and excreted as diarrhea, which is sometimes foul-smelling.
This alternation of constipation (constipation) and diarrhea (diarrhea) is also known as paradoxical diarrhea. It is a classic warning sign of colon cancer.
Some people just have repetitive constipation or diarrhea.
If stool is inadvertently excreted when passing diapers, this can also be an indication of colon cancer. Doctors speak here of the phenomenon of the "false friend".
It occurs when the muscle tension of the anal sphincter is decreased. The reason for this can be deep-seated colon cancer that affects the muscle and disrupts its function.
Sometimes bowel cancer just changes stool shape. It then appears about as thin as a pencil. This is what the term “pencil chairs” is based on.
In people over 40 years of age, any change in bowel habits that lasts over three weeks should be discussed with a doctor.
Blood in the stool
A malignant tumor bleeds easily. In colon cancer, this blood is excreted with the stool. In the majority of colon cancer patients, for example, blood is found in the stool.
-
Use colon cancer screening!
Three questions for
Dr. med. Uta Plat,
Specialist in internal medicine -
1
Is there a good way to prevent colon cancer?
Dr. med. Uta Plat
In any case! Much can be achieved through diet. It should be high in fiber and contain plenty of fruits and vegetables. In addition, you should only consume a little dark red meat and smoked goods. Also helpful: reduce alcohol, do not smoke, take part in regular sports, lose excess weight. And: Use the preventive measures for colon cancer, especially the colonoscopy - the so-called preventive colonoscopy.
-
2
How often should you have colon cancer screening?
Dr. med. Uta Plat
The screening colonoscopy is recommended from the age of 55 at intervals of ten years. In the event of complaints, hereditary risk or if polyps have been removed, the mirror should definitely be done at shorter intervals. A stool test for occult (invisible) blood is carried out during the annual preventive medical check-up from the age of 50. But this test is unsafe! Even if no blood is found, a colonoscopy should follow if in doubt.
-
3
Why are so many afraid of a colonoscopy?
Dr. med. Uta Plat
The colonoscopy is now a routine examination. Preparing to cleanse the bowel, which has to be completely emptied, is somewhat uncomfortable. But this is absolutely necessary so that we do not overlook anything. The actual colonoscopy is then usually carried out in twilight sleep so that the patient does not notice anything. Since helium gas has been used to unfold the intestine, massive flatulence no longer occurs after the examination.
-
Dr. med. Uta Plat,
Specialist in internal medicineSenior physician at the Paracelsus Clinic "Am Schillergarten" in Bad Elster, since 2009 in the oncology department.
Visible blood
This blood is sometimes visible to the naked eye. If the colon cancer is in the rectum, the blood in the stool appears bright red (fresh blood). If the cancer grows earlier in the colon, the blood appears dark red.
Black stools (tarry stools) indicate bleeding in the upper digestive tract (stomach, duodenum).
Occult blood
However, many colon cancer patients excrete so little blood that it is not immediately noticeable in the stool. These "invisible" additions of blood are also known as occult blood. It can be detected with certain tests (for example hemoccult test).
Other causes of bloody stool
Blood in your stool is not a specific sign of colon cancer. Most of the time, blood residues on the stool or toilet paper are due to hemorrhoids. Typically, the blood is then rather bright red and deposited on the stool. The blood in colon cancer, on the other hand, is often mixed with the stool due to bowel movements.
Various intestinal infections or chronic intestinal inflammation can also cause bloody stools.
Inefficiency and fatigue
Colon cancer can also cause a person's general condition to deteriorate. For example, those affected feel unusually tired and weak and are not as productive as usual. A fever can also be a sign of colon cancer.
Anemia
Anemia can occur particularly in the advanced stages of the disease. It occurs because the malignant colon tumor often bleeds. Anemia manifests itself with symptoms such as paleness, poor performance, tiredness and, in severe cases, shortness of breath.
Weight loss
Another sign of colon cancer at an advanced stage is unwanted weight loss. Colon cancer removes additional energy from the body. Patients lose weight as a result, even if they continue to eat as usual.
Intestinal obstruction
Colon cancer can always grow in the intestine. A large tumor, for example, can constrict the intestine so that the remains of food can no longer pass through the site. This creates an intestinal obstruction (ileus) - a serious complication of colon cancer.
pains
Pain can also occur with colon cancer, for example cramping abdominal pain. Some patients also have painful bowel movements.
Peritonitis
If the tumor continues to grow, it can break through the intestinal wall and cause peritonitis. Sometimes colon cancer also grows in neighboring organs, such as the urinary bladder.
If the cancer cells spread in the abdominal cavity on the peritoneum, doctors speak of peritoneal carcinosis.
Metastases
If the colon cancer has spread to other parts of the body (metastasis), further symptoms can occur. Usually it forms daughter tumors in the liver (liver metastases). This can cause pain in the upper right abdomen, jaundice or increased liver values in the blood, for example.
Lung metastases are also possible in colon cancer. You can make yourself noticeable by breathlessness or coughing, for example. Metastases are less common in the skeleton or in the brain.
Colon cancer: rectal cancer
The rectum or rectum is the end piece of the large intestine. If a malignant tumor forms here, doctors speak of rectal cancer.
Rectal cancer is usually removed surgically. Depending on the tumor stage, patients also receive radiation therapy and / or chemotherapy.
Read more about this form of colon cancer in the article rectal cancer.
This is how the large intestine is built
Colon cancer: causes and risk factors
In most cases, colon cancer arises from benign growths of the intestinal mucosa. For many people, these so-called intestinal polyps remain harmless. In others, however, they develop into colon cancer.
Intestinal polyps usually arise from the glandular tissue of the intestinal wall. This makes them one of the so-called adenomas. Colon cancer that develops from such benign adenomas is classified as adenocarcinoma (carcinoma = cancerous tumor).
Colon polyps as a risk factor for colon cancer
Adenoma-carcinoma sequence
Colon cancer develops slowly. It usually takes years for healthy intestinal mucosa to develop into an adenoma and even degenerate cancer.
Doctors call this process adenoma-carcinoma sequence or serrated carcinogenesis pathway. The size, number and tissue structure of the adenomas determine the risk of colon cancer.
Risk factors for colon cancer
According to the current state of knowledge, colorectal cancer is triggered by various risk factors. Certain dietary and lifestyle habits as well as hereditary factors are among the possible causes of colorectal cancer.
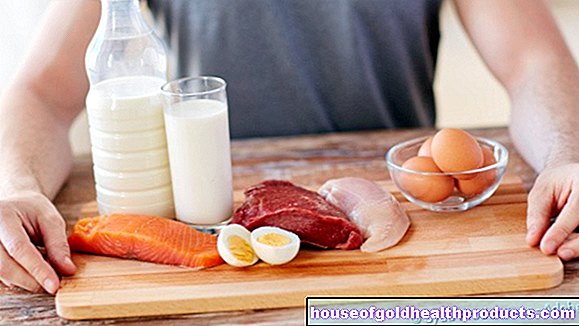
Diet and lifestyle
A low-fiber, high-fat, meat-based diet (particularly high levels of red meat and processed sausages) increases the risk of colon cancer. This food passes through the intestine more slowly than vegetable, fiber-rich food. Carcinogenic substances from food stay in contact with the intestinal mucosa for longer and can damage it, experts suspect.
A lack of exercise and obesity also promote the development of colon cancer. Alcohol and nicotine also increase the risk of colorectal cancer (and other cancers).
Genetic factors
It can be observed that first-degree relatives (parents, children, siblings) of colorectal cancer patients are more likely to develop this type of cancer themselves than other people. So is colon cancer hereditary? Who is at increased risk? Then what is important?
Genetic predisposition
For one thing, there is obviously a genetic predisposition. However, researchers cannot discover any definite changes in the genetic make-up. But not everyone who has relatives with colon cancer will develop it themselves. Most often the combination of genetic makeup and lifestyle triggers colon cancer.
If colon cancer accumulates in a family, first-degree relatives such as siblings and children have a two to three times higher risk of developing colon cancer themselves. If a first-degree relative falls ill before the age of 60, this risk even increases three to four times.
“Increased risk” does not mean that those affected will definitely get colon cancer!
Colon polyps in the family also play a role. If doctors found such in first-degree relatives before they were 50, your own risk of colon cancer is also increased.
Second-degree relatives, on the other hand, (grandchildren, grandparents, cousins and their parents) have only a slightly increased risk of colon cancer. However, exact figures are not yet known.
As far as we know, third-degree relatives no longer have an increased risk of colon cancer.
Talk to your relatives openly about previous illnesses in the family! This is the only way you and your relatives can recognize a possible risk of colon cancer!
Hereditary colon cancer
However, there are detectable gene changes (mutations) that directly promote the formation of a malignant tumor in the intestine. The two most well-known hereditary diseases of colon cancer are:
- HNPCC (Hereditary Non-Polyposis Colon Cancer or Lynch Syndrome): This is the most common type of hereditary colon cancer. Due to mutations, various repair systems for the genetic material are defective here. Faulty cells are formed more often. This significantly increases the risk of colon cancer, as well as that of other cancers (such as uterine, ovarian and stomach cancer).
- FAP (familial adenomatous polyposis, FAP): In this rare disease, countless polyps form throughout the intestine at a young age.If left untreated, they almost always develop into colon cancer. Often, as a precautionary measure, sections of the intestine are surgically removed to prevent colon cancer in FAP.
Those affected fall ill with these hereditary diseases much earlier than usual. Doctors advise everyone suspected of having HNPCC to have an annual colonoscopy from the age of 25. Doctors even examine people with FAP once a year from the age of ten and remove abnormal polyps.
Age as a risk factor
Age also has a big influence: the older someone is, the higher their risk of colon cancer. About 90 percent of all colon cancers occur after the age of 50. More than half of colorectal cancer patients are older than 70 years.
Chronic Inflammatory Bowel Disease
Colon cancer risk is also increased if someone has inflammatory bowel disease. People with ulcerative colitis are particularly affected: their colon is chronically inflamed. About five percent of those affected develop colon cancer.
The risk of colon cancer can also be increased with Crohn's disease. This is especially true if the chronic inflammation affects the large intestine (but it is usually limited to the last section of the small intestine).
Type 2 diabetes mellitus
People with type 2 diabetes (type 2 diabetes mellitus) have increased levels of the messenger substance insulin in their blood in the early stages of the disease. According to some researchers, these are responsible for the fact that the risk of colon cancer is significantly increased. Insulin apparently promotes the growth and multiplication of cells in general - including cancer cells.
Colon cancer: examinations and diagnosis
Every year around 29,500 women and 33,500 men develop colon cancer. At diagnosis, the average age of the patients is 71 years (men) and 75 years (women).
If you suspect colon cancer, you should first contact your doctor. If a colonoscopy makes sense, he will refer you to a gastroenterologist.
The doctor will first talk to you in detail to collect your medical history (anamnesis). He will have your complaints described in detail. He will also collect information that will help him better assess the likelihood of you having colon cancer. Possible questions from the doctor in the anamnesis interview are:
- Has your digestion changed (e.g. constipation or diarrhea)?
- Have you noticed any traces of blood in your stool?
- Does your family already have colon cancer?
- Does anyone in your family have or have had other cancers such as breast, ovarian or cervical cancer?
- Have you lost weight by accident?
- Do you smoke and drink alcohol?
- How often do you eat meat?
- Do you have any known diabetes?
Physical examination
Next, the doctor will examine you: Among other things, he will listen to your stomach with the stethoscope and palpate it with his hands. In colorectal cancer, the palpation exam can sometimes be painful.
An important examination for suspected colon cancer is the so-called digital rectal examination (DRE). The doctor inserts his finger into the anus and feels the end of the intestine with his finger. A colon cancer sitting there can be easily felt in this way (hard, bumpy). Sometimes the doctor also recognizes blood residues on the glove after a DRE.
Up to ten percent of colon cancer can be palpated this way!
Test for blood in the stool
Sometimes a stool sample is used to check whether there is blood in the stool that is not visible to the naked eye (occult blood). This test is called a fecal occult blood test (FOBT).
However, FOBTs do not tell you exactly where in the gastrointestinal tract there is bleeding. The test can also be positive if blood is swallowed, for example if there is bleeding from the nose or gums.
Conversely, not all colon tumors bleed - or at least not all the time. Even if the test is negative, there may be cancerous tumors in the intestine (false negative result). A colonoscopy is therefore always the safer alternative.
Immunological stool test (i-FOBT)
For some time now, doctors have been using the so-called immunological stool test (i-FOBT). He can differentiate between human and animal blood (when consuming raw meat) in the stool. This is done with the help of antibodies that only bind to human blood.
You can get the test from your general practitioner or gastroenterologist. It contains a spatula, a toilet catcher and a tube. You fill a stool sample into the tube and give it to your doctor. He sends the test to a laboratory for examination.
A stool sample is usually sufficient for an immunological stool test.
Women should not do the stool immunological test during or shortly after their period. This can lead to a false positive test result.
You can read more about the test and its accuracy in the article Immunological stool test (iFOBT).
Hemoccult test
The hemoccult test that was used in the past has now been largely replaced by the immunological stool test.
He also jumps on animal blood and some vegetables. For example, patients who eat raw meat before taking a sample receive a false-positive result.
Whether immunological stool test or haemoccult test: If colon cancer is suspected, a colonoscopy is also carried out.
More stool tests
There are other tests that check the stool for signs of colon cancer. For example, the M2-PK test looks for a specific protein that is associated with the tumor. Current medical guidelines do not recommend the use of this test.
Genetic or DNA stool tests look specifically for colon cancer cells - based on their genetic makeup. The studies suggest a benefit, but the data are insufficient to make a recommendation. In addition, this test is very expensive in comparison.
Colonoscopy
It is the most informative examination for suspected colon cancer. Specialized doctors (gastroenterologists) examine the intestine with a tubular instrument (endoscope) that is equipped with a small camera and a light source. The endoscope is inserted into the intestine. The inside of the intestine is then viewed on a monitor.
As part of the colonoscopy, the doctor can remove suspicious colon polyps directly. It is also possible to take tissue samples (biospies) from suspicious areas of the intestinal mucosa. You will then be examined histologically. In this way, colon cancer can be reliably detected or excluded.
You can read more about the examination procedure in the article Colonoscopy.
Virtual and small colonoscopy
If a normal colonoscopy cannot be performed, the doctor can switch to a virtual colonoscopy or a rectoscopy / sigmoidoscopy.
Virtual colonoscopy
In a virtual colonoscopy (CT or MR colonography), computed tomography (CT) or magnetic resonance imaging (MRI) provide many images of the intestine. A computer calculates a three-dimensional image from them and displays it graphically.
Here, too, the patient must completely empty his bowel beforehand using laxatives (like a normal colonoscopy).
A disadvantage of the virtual colonoscopy is that the result is not as precise as with a normal colonoscopy. In addition, polyps cannot be removed or tissue samples taken during the examination. A proper colonoscopy or surgery may be necessary afterwards.
Recto-sigmoidoscopy (small colonoscopy)
Rectoscopy is the reflection of the rectum with an endoscope. With sigmoidoscopy, the doctor examines not only the rectum but also the section of intestine in front of it (S-shaped colon loop). In contrast to a normal colonoscopy, the doctor does not examine the entire colon with this "small" colonoscopy.
Further investigations in colon cancer
Once the diagnosis of colon cancer has been made, further examinations must show how far the cancer has progressed (colon cancer stages: see below). Doctors speak of so-called "staging":
- Rectal ultrasound examination (sonography): This can be used to determine how far the tumor has already spread in the intestinal wall.
- Ultrasound examination (sonography) of the abdomen: With the ultrasound, the doctor looks for subdivisions (metastases), especially in the liver. He can also examine other abdominal organs (spleen, kidneys, pancreas).
- Computed tomography (CT): Here too, the doctor looks for colon cancer metastases, for example in the lungs or liver. In order to better differentiate individual structures from one another, the doctor will administer a contrast medium (contrast medium) before the examination.
- Magnetic resonance tomography (magnetic resonance tomography, MRT): MRI with contrast media allows a very precise representation of various tissues and organs - more precisely than with CT. The MRI is especially important before an operation.
- X-ray of the chest: A chest X-ray helps to track down daughter settlements (metastases) in the lungs. Compared to CT or MRI, however, it is rather imprecise.
Tumor markers
In colon cancer patients, the doctor regularly measures so-called tumor markers in the blood. Tumor markers are substances that are found to a greater extent in the blood of many cancers.
In colon cancer, the "carcinoembryonic antigen" (CEA) in particular can be increased in the blood. However, it is not suitable for the early detection of colon cancer. This is because healthy intestinal cells also produce CEA, and the value can also be increased in smokers and liver diseases. Rather, the CEA level helps to assess the course of the disease and the success of the therapy.
After the tumor has been surgically removed, the CEA values usually drop to the normal range. If there is a relapse (relapse), the value rises again. The effect of chemotherapy can also be assessed at the CEA.
Doctors determine the CEA value even after successful therapy - as part of follow-up care. In this way, a relapse can often be recognized at an early stage!
Genetic counseling
If hereditary colon cancer (HNPCC, FAP and other rare forms) is suspected, genetic counseling and examination is usually carried out. Those affected turn to specialized centers. The expert then examines the patient's genetic makeup for characteristic genetic changes (mutations).
If the doctor discovers a hereditary tendency to colon cancer, he also offers close relatives (parents, siblings, children) genetic counseling and a genetic test. In addition, the doctor can recommend further, individual colon cancer screening. This depends on the cause:
- Genetic predisposition without evidence of hereditary changes: First mirror ten years before the age of onset of the affected first-degree relative, at the latest from the age of 40-45, if the findings are normal, repetition every ten years
- Suspected HNPCC: mirroring at least every three (to five) years, genetic counseling from the age of 25
- Secure HNPCC: Annual colonoscopy from the age of 25, from the age of 35 also gastroscopy; For women aged 25 and over, an additional annual gynecological ultrasound examination for early detection of ovarian and uterine cancer; From the age of 35 samples are taken from the uterine lining.
- Suspected / confirmed FAP: genetic counseling from the age of ten, from then on also annual recto-sigmoidoscopy; in the case of adenomas, extension to complete colonoscopy
Colon cancer stages
Two systems are common for the staging of colon cancer: First there is the so-called TNM classification. It can be used for almost all tumors and describes the spread of the tumor. Using the TNM classification, the cancer can then be divided into certain bowel cancer stages according to the UICC (Union internationale contre le cancer).
TNM classification
TNM is an abbreviation for the following three terms:
- T for tumor: This parameter indicates the spread of the tumor. It is based on the so-called infiltration depth (i.e. how deep the tumor has penetrated into the tissue).
- N for nodes (lymph nodes): This parameter indicates whether and how many lymph nodes are affected by the cancer cells.
- M for metastases (daughter tumors): This factor indicates whether and how many metastases are present in more distant body regions.
A numerical value is assigned for each of these three categories. The more advanced the disease, the greater the numerical value. The TNM classification in colorectal cancer is:
|
Tis |
Carcinoma in situ |
Carcinoma in situ (CIS) is an early form of colon cancer. The colon cancer is still in the top layer of tissue (epithelium). |
|
T1 |
Involvement of the submucosa |
The tumor has spread to the thin layer of connective tissue (submucosa) below the intestinal mucosa. |
|
T2 |
Involvement of the muscularis propria |
The tumor extends even further into the muscle layer below the submucosa. |
|
T3 |
Invasion of the subserosa and the pericolic or perirectal adipose tissue |
The tumor has attacked all layers of the wall of the intestine and extends to the outer layer of connective tissue (subserosa) or to the adjoining fatty tissue. |
|
T4 |
Infiltration of the peritoneum (T4a) or other organs / structures (T4b) |
The tumor has also affected the peritoneum or other organs. |
|
N0 |
No lymph node involvement | |
|
N1 |
1-3 regional lymph nodes |
Regional lymph nodes are the lymph node station near the tumor |
|
N2a |
4-6 regional lymph nodes | |
|
N2b |
≥7 regional lymph nodes | |
|
M0 |
No distant metastases | |
|
M1a |
Distant metastases: only one organ affected |
A so-called peritoneal carcinosis is an extensive infestation of the peritoneum (peritoneum) with cancer cells. |
|
M1b |
Distant metastases: more than one organ affected or peritoneal carcinoma |
Colon cancer stages according to UICC
The UICC (Union internationale contre le cancer) colorectal cancer stages are based on the TNM classification. Depending on the extent of the tumor infestation, colorectal cancer is assigned to a specific UICC stage in each patient. The treatment is then based on this. In addition, the patient's prognosis can be roughly estimated using the UICC stage.
Examples: A patient with an advanced tumor (T4) according to the TNM classification is still in UICC stage II as long as there are no daughter settlements in lymph nodes or other organs (N0, MO). On the other hand, a patient with a proven distant metastasis (M1) is always in the most severe colorectal cancer stage IV.
Here is an overview of all UICC colon cancer stages:
|
UICC stage: |
TNM classification |
|
0 |
Tis |
|
I. |
to T2 if N0 and M0 |
|
II |
T3 to T4 if N0 and M0 |
|
III |
every T at N1 or N2 and M0 |
|
IV |
every T and every N if M1 |
Colon cancer: treatment
If colon cancer is discovered in good time, i.e. before it has formed daughter settlements in the body, it can often be cured. The exact therapy for colon cancer depends initially on which section of the intestine is affected.
There are fundamental differences between the treatment of colon cancer and that of rectal cancer. This section of text explains the treatment of colon cancer.
You can find out how rectal cancer is treated in the text rectal cancer.
The exact treatment plan for colon cancer depends on several factors: It matters where exactly the tumor is located, how big it is and whether it has already spread to other parts of the body (tumor stage). The patient's age and general condition also influence therapy planning.
Colon cancer: surgery
The main treatment for colon cancer is surgery: surgeons cut out the affected part of the colon.
The surgeon then sews the remaining intestinal ends together. So the patient has a continuous bowel again. In colon cancer, an artificial anus (anus praeter, stoma) only has to be created permanently or temporarily.
Lymphadenectomy
Along with the affected section of the intestine, the adjacent lymph nodes are also removed. Pathologists examine the intestinal section and lymph nodes under the microscope. In the case of intestinal tissue, one checks whether the tumor has been completely excised. When the lymph nodes are removed, the doctors check whether cancer cells have already spread there.
Colon cancer surgery for metastases
Even at more advanced stages, doctors try to treat colon cancer surgically. They also cut out daughter tumors such as lung or liver metastases. The prerequisite, however, is that the location and number of the metastases and the general condition of the patient allow this procedure.
Chemotherapy for colon cancer
If the colon cancer is more advanced, many patients receive chemotherapy in addition to surgery. The danger here is that individual cancer cells have already spread throughout the body. Chemotherapy aims to kill these cancer cells.
Doctors call chemotherapy after the operation adjuvant chemotherapy. In addition, doctors treat metastatic colon cancer with chemotherapy, especially if they cannot operate on the colonies.
The patient receives special cancer drugs, so-called cytostatics. They inhibit the growth of cancer cells or damage them directly, causing them to perish.The cytostatics are administered at regular intervals either as an infusion and / or in tablet form. The duration of therapy extends over about half a year.
You can find out more about the course of the therapy in the article Chemotherapy
Immunotherapy for colon cancer
In some cases of advanced colon cancer, doctors add immunotherapy to chemotherapy. Special antibodies are used, which are directed against specific features of the tumor.
Immunotherapy for cancer is therefore particularly suitable for patients whose tumor has precisely these characteristics. To do this, doctors (pathologists) test the genome of colon cancer for various genetic changes (e.g. RAS, BRAF, microsatellite status) as part of a so-called molecular pathological examination.
EGF receptor antibodies
For example, in colon cancer, doctors use EGF receptor antibodies (such as cetuximab or panitumumab). They occupy the docking sites (receptors) for the epidermal growth factor (EGF) on the cancer cells. The growth factor can no longer dock - tumor growth is slowed down.
VEGF antibodies
Another immunotherapy includes VEGF antibodies (such as bevacizumab): The "vascular endothelial growth factor" (VEGF) actually ensures that new blood vessels are formed (angiogenesis) and supply the tumor with nutrients and oxygen.
The antibodies inhibit VEGF and thus prevent the formation of new blood vessels supplying the tumor (angiogenesis inhibitors). Colon cancer is therefore no longer receiving enough blood to be able to spread any further.
Radiation therapy for colon cancer
Radiation therapy plays a role in colorectal cancer, especially if the tumor is located in the rectum (rectal cancer).
In contrast, it is not common in colon cancer. At most, it can be useful to specifically combat metastases in bones or the brain, for example.
Therapy of liver metastases
Colon cancer is common in colon cancer. Doctors usually try to surgically remove these metastases. But that is not always possible. Then other methods can be used. These include above all radio frequency ablation (RFA) and selective internal radiation therapy (SIRT).
You can read more about liver metastases and their therapy in our article Liver metastases.
alternative medicine
Mistletoe therapy is widespread. However, their effect has not been proven; studies on this are mostly of poor quality. The few good studies show no influence on a tumor disease such as colon cancer.
Green tea extracts could prevent relapses. At least that's what a small study shows. Other herbal substances showed only minor effects in the laboratory.
Rather, the experts in the guidelines point out that virtually all alternative colon cancer remedies have no scientific basis and are expensive. Plant-based products from Asia in particular are repeatedly contaminated (heavy metals, pesticides, etc.).
Homeopathy in general has no scientifically proven specific effect on colon cancer.
Look out for “miracle cures” and treatment methods that are supposedly free of side effects. These offers are mostly dubious and do more harm than good.
Colon cancer: disease course and prognosis
The course of the disease and the prognosis of colorectal cancer depend crucially on the stage of the disease. In principle, doctors always try to cure colon cancer (curative treatment). Sometimes, however, they can only delay the progression and the associated complications with therapy, but cannot prevent death (palliative treatment).
Follow-up examinations
After the curative treatment, the doctor creates an individual follow-up plan over a period of five years. In this context, the patient receives special follow-up examinations.
They include, for example, a doctor-patient conversation, a physical examination, the determination of the tumor marker CEA in the blood, a colonoscopy (colposcopy), ultrasound examinations of the abdomen and, if necessary, computed tomography. When which examination is due, the patient can find out from his doctor.
Colon Cancer: Chances of a Cure
Whether colon cancer is curable depends crucially on the stage of the disease. Discovered and treated at an early stage, it is easily curable. However, the more advanced the tumor is, the lower the chances of a cure for colon cancer.
In the case of extensive infestation of the peritoneum (peritoneal carcinosis), the mean survival time of the patient is even lower than in the case of other metastases (for example in the liver).
Colon cancer: life expectancy
The life expectancy of colon cancer patients has increased in recent years. On the one hand, this is due to the screening program: From a certain age, regular colon cancer screening examinations are provided. Colon cancer is often discovered in its early stages. On the other hand, improved treatment options also increase the life expectancy of colon cancer patients.
In general, colon cancer life expectancy depends on the stage of the disease. It is usually given with the so-called five-year survival rate. This is the proportion of patients who are still alive five years after diagnosis.
The prerequisite for this, of course, is that treatment has taken place. For colon cancer and rectal cancer, the five-year survival rates are approximately:
|
UICC stage: |
Colon cancer |
Rectal cancer |
|
I. |
95 percent |
95 percent |
|
II |
90 percent |
85 percent |
|
III |
65 percent |
55 percent |
|
IV |
5 percent |
5 percent |
Please note that these are statistical mean values. The prognosis in individual cases can sometimes differ considerably from these values.
Colon cancer: terminal stage
Those affected with colon cancer in the highest stage (stage IV) unfortunately have a very poor prognosis. In this situation, healing (curative therapy approach) is usually no longer possible. The patients then receive palliative treatment.
Above all, it aims to alleviate the patient's symptoms and thus improve his quality of life. With palliative chemotherapy, doctors also try to delay the progression and further suffering as long as possible. Colon cancer patients must be aware, however, that chemotherapy cannot cure them.
Colon cancer screening
Colon cancer often only causes symptoms when it has progressed further. Then the chances of a cure are no longer as good as in the early stages of cancer. That is why preventive medical checkups are very important. This is especially true if someone has known risk factors for colorectal cancer such as overweight or increased or early colon cancer in the family.
As part of the statutory bowel cancer check-up, the health insurance companies pay for certain examinations at certain intervals for patients aged 50 and over. These include, for example, an examination of the stool for "hidden" (occult) blood and a colonoscopy.
You can find out when you are legally entitled to such colon cancer screening examinations in the article Colon cancer screening.
Factors protecting against colon cancer
In addition to the risk factors for colon cancer mentioned, there are also influencing factors that protect against colon cancer. This includes regular physical activity and a high-fiber, low-meat diet. The exercise and fiber stimulate bowel movements. The food remains are transported through the intestine more quickly. This means that toxins in the stool can act less long on the intestinal mucosa - the risk of colon cancer is reduced.
Additional information
You can find more information about colon cancer and colon cancer screening on the Felix Burda Foundation website (www.felix-burda-stiftung.de)
Guidelines:
- Guideline "Colorectal Carcinoma" of the German Society for Gastroenterology, Digestive and Metabolic Diseases
- Patient guideline "Early detection of colon cancer" of the German Society for Gastroenterology, Digestive and Metabolic Diseases
- Patient guideline "Colon cancer in the early stages" of the German Society for Gastroenterology, Digestive and Metabolic Diseases
- Patient guideline "Colon cancer in the advanced stage" of the German Society for Gastroenterology, Digestive and Metabolic Diseases
Self-help groups:
- Deutsche ILCO e.V. - Nationwide organized self-help association of ostomists and people with colon cancer: https://www.ilco.de/
- German Cancer Aid: https://www.krebshilfe.de/




.jpg)