Thrombic endarterectomy
All content is checked by medical journalists.A thrombendarterectomy is a procedure used to surgically reopen blocked blood vessels. In addition to the blood clot, part of the blood vessel is also removed. The arteries in the neck and groin are often affected. Read all about the surgical procedure, when it is performed, and the risks involved.

What is a thrombus endarterectomy?
Thrombendarterectomy (TEA) is a surgical procedure to open blood vessels that have been blocked by a blood clot (thrombus). The surgeon removes not only the thrombus, but also the inner wall of the artery. After a thrombus endarterectomy, the blood flows back into parts of the body that were not or no longer supplied with blood due to the blockage.
Thrombendarterectomy is divided into three types:
- Direct (open) thrombus endarterectomy
- Indirect closed thrombus endarterectomy
- Indirect semi-closed thrombus endarterectomy
When is a thrombus endarterectomy performed?
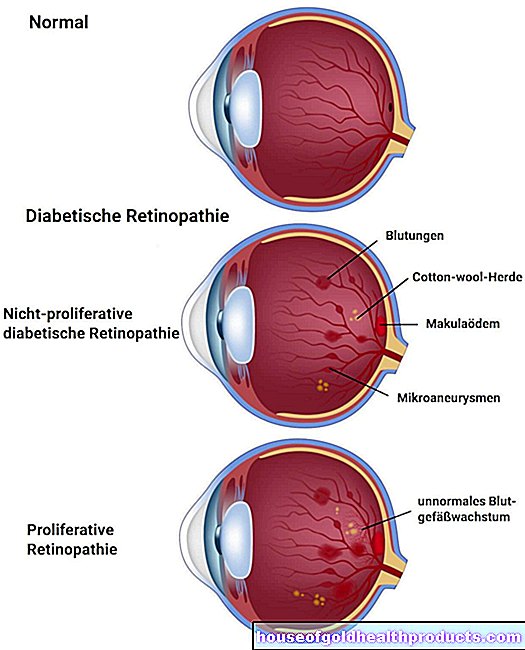
Surgeons perform a thrombus endarterectomy for narrowing or occlusion of arteries. Risk factors for vascular diseases in which such a narrowing can occur due to deposits in the vessels (arteriosclerosis) include smoking, high blood pressure and diabetes. In addition, blood clots often form on the inner walls of the arteries, preventing the blood from flowing through. Some vessels, such as the arteries in the neck and groin, are particularly often affected.
Carotid artery
If a long length of the carotid artery is narrowed, vascular surgeons may consider thrombendarterectomy. Other treatment options are the insertion of so-called stents - vascular supports made of metal or synthetic fibers - which keep the blood vessel open or the replacement of the diseased carotid artery segment with an artificial vessel.
Arteries
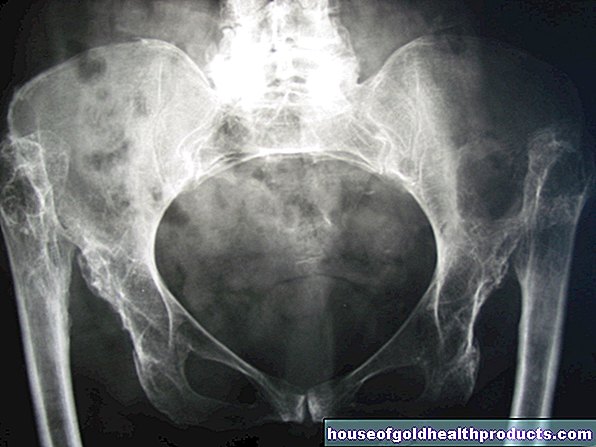
In so-called peripheral arterial occlusive disease (PAD), the femoral arteries are often affected by a sudden vascular occlusion caused by a blood clot. Due to the lack of blood flow, the leg below the constriction can die because it is no longer adequately supplied with blood. The arteries in the hollow of the knee or in the lower legs are also often affected. Depending on the extent of the constriction, in addition to thrombus endarterectomy, bypass surgery is suitable for treatment.
Intestinal arteries
The arteries of the intestine are usually closed by migrating thrombi (embolus). The patients here suffer from severe abdominal pain, among other things. A thrombus endarterectomy on the affected arteries helps preserve the bowel.
Other blood vessels that surgeons often perform thrombendarterectomy are the pelvic arteries, the arteries near the heart, and the arteries of the arm.
What do you do with a thrombus endarterectomy?
Before the actual operation, the attending surgeon thoroughly examines the vessel in question. In addition to ultrasound, X-ray examinations or magnetic resonance imaging are available for this purpose.
The procedure itself is usually carried out under general anesthesia, but local anesthesia is often sufficient. After the surgeon has washed, disinfected and covered the surgical area with sterile material, he cuts the skin with the scalpel. Depending on which form of thrombus endarterectomy is chosen, the incisions differ.
Direct thrombendarterectomy
Here the surgeon completely opens the affected blood vessel section and the skin over it. With a surgical instrument (spatula), he removes the blood clot along with the inner layer of the arteries. To prevent a new narrowing, the surgeon often sews a piece of another vessel into the previously narrowed area. This so-called patch significantly increases the diameter of the artery.
Indirect thrombendarterectomy
In indirect thrombus endarterectomy, the narrowed vessel is cut open either on one side of the constriction (closed thrombus endarterectomy) or on both sides (half-closed thrombus endarterectomy). The surgeon inserts an instrument through the opening to remove the thrombus.
After the artery is permeable again, the corresponding part of the body is x-rayed and checked whether the constriction has been removed.
What are the risks of a thrombus endarterectomy?
A thrombendarterectomy is a complex surgical procedure with all the risks of an operation. Despite the sterile working method and the preventive administration of antibiotics, the tissue can become infected with germs. Bleeding can also occur during or after the thrombus endarterectomy. Depending on the severity of the complications, another procedure may be necessary.
In general, only arteries over five millimeters in diameter are large enough for thrombus endarterectomy. With smaller blood vessels, the risk of re-narrowing after the operation is significantly higher.
Nerve damage
Nerves that can be injured during the operation often run alongside the arteries. Typical symptoms are then sensation disturbances, numbness or paralysis. These are not always permanent, but usually require extensive treatment.
Bleeding in other parts of the body
To prevent the operated blood vessel from closing again, the doctor will administer various blood-thinning medications. These increase the risk of serious bleeding. If the brain is affected, a stroke can result.
Contrast agent allergy
Before the X-ray of the surgical area, the doctor injects an X-ray contrast agent that makes the blood vessels visible and can trigger allergic reactions. Depending on the severity of the allergic reaction, medication that supports the circulation and inhibits allergies are given.
Additional measures
If a thrombus endarterectomy is insufficient to restore blood flow, other procedures are used. These include, for example, the introduction of a stent that keeps the artery open or a bypass operation.
What should I watch out for after a thrombendarterectomy?
Tell your doctor if you suddenly have pain in the wound area or the dressing is bloody after a thrombendarterectomy. You must also urgently report numbness or paralysis, as these indicate a renewed closure or nerve damage.
Following a thrombendarterectomy in the leg area, you should elevate the leg and wear compression stockings. This prevents swelling in the area of the wound. During personal hygiene, the wound must not get wet and should be protected with special plasters. In the first few weeks after the procedure, you should also refrain from bathing in full baths or going to the swimming pool so that the wound does not become infected.
To strengthen the muscles, you will make your first attempts to walk soon after the thrombendarterectomy, later you can also cover longer distances with physiotherapeutic help.
Tags: smoking elderly care sports fitness







.jpg)