Fundoscopy
Markus Fichtl is a freelance writer in the medical department.
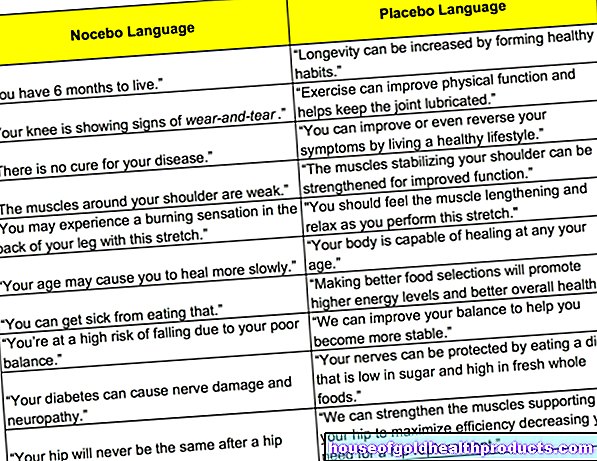
More about the experts All content is checked by medical journalists.In fundoscopy (fundoscopy, ophthalmoscopy), the fundus is examined for changes with the help of various instruments. In this way, various eye diseases can be diagnosed and their therapy planned. A distinction is made between direct and indirect ophthalmoscopy. Read here what exactly is meant by this, how a funduscopy works and when it is carried out!

What is a funduscopy?
In fundoscopy (fundoscopy, ophthalmoscopy), the fundus is examined using various mirrors with an electric light source and magnifying glasses. In this way, the ophthalmologist can look directly at pathological changes in the choroid, retina and optic nerve. There are several techniques for an ophthalmoscope:
Direct ophthalmoscopy (mirroring in the upright image)
In direct ophthalmoscopy, the light from a lamp is reflected onto the back of the patient's eye. To do this, the doctor holds an ophthalmoscope close to the patient's eye to be examined. The examiner can view the eye fundus illuminated in this way in the upright image as if through a keyhole through the patient's pupil at a magnification of around 16x. By interposing various lenses, both ametropia of the doctor and / or patient can be compensated so that the examiner receives a sharp image of the fundus.
This type of fundus examination offers a good opportunity to detect even small retinal changes due to the high magnification. However, only a small section of the fundus can be viewed and only a two-dimensional image is obtained.
Indirect ophthalmoscopy (mirroring in the reverse image)
In contrast to direct ophthalmoscopy, with the indirect technique, the light reflected on the patient's ocular fundus is viewed through a converging lens (magnifying glass). The examiner therefore sees a virtual image that is created a few centimeters in front of the patient's eye, is upside down and reversed.
This type of fundoscopy is often referred to as the ophthalmologist's "standard method". Compared to the direct method, it offers a significantly lower magnification (two to six times), but a better overview of the entire fundus. In particular, the periphery of the retina can be seen better with indirect ophthalmoscopy. With special systems, the examiner can even look into the patient's eye with both eyes, which makes it easier to assess abnormalities spatially.
Contact glass examination
With this variant, the fundus examination is carried out on the slit lamp. First, the eye to be examined is anesthetized with special eye drops, then a protective gel is applied to the cornea. Then a magnifying glass (contact glass) is placed directly on the eye.The examination of the fundus through the contact glass then takes place together with the slit lamp.
The combination of slit lamp and contact glass gives a greatly enlarged three-dimensional fundus image and still a good overview of the entire fundus and the corner of the anterior chamber. The latter is important for diagnosing glaucoma. The contact lens examination thus combines the advantages of direct and indirect ophthalmoscopy, which makes it the gold standard in the diagnosis of retinal diseases.
When is a funduscopy performed?
Basically, a funduscopy is always necessary when the doctor has to assess the fundus. This includes the entry point of the optic nerve, the macula (“yellow spot”, the place of sharpest vision), retinal vessels and the retina itself and its periphery. For example, a funduscopy is performed for the following reasons:
- for diagnosis or monitoring of changes in the eyes caused by diabetes mellitus (diabetic retinopathy), high blood pressure or arteriosclerosis
- for the diagnosis or follow-up of age-related macular degeneration (most common cause of severe visual disturbances in old age)
- if there is any suspicion of occlusion or malformation of one or more retinal vessels
- if a retinal detachment is suspected
- for diagnosing or monitoring the progress of retinal tumors such as retinoblastomas
What do you do with a funduscopy?
First, the pupil of the eye to be examined is dilated using an anticholinergic drug (such as tropicamide) in order to enable an optimal view. Before doing this, it must be ensured that there is no flat anterior chamber in the eye, otherwise there is a risk of a so-called "angle block". The drainage of the aqueous humor is made more difficult, which can increase the intraocular pressure. Retinal damage is the possible consequence.
The actual funduscopy is then carried out. The fundus is searched systematically, area by area. Any changes are documented by means of a sketch. This later forms the basis for further therapy planning.
In the contact glass examination - as mentioned above - the eye is initially locally anesthetized with drops and a protective gel is applied to the cornea.
What are the risks of a funduscopy?
Performing a funduscopy is largely risk-free. In very rare cases, the following complications can occur:
- Inflammation
- Infections
- Side effects of the anticholinergic drug to dilate the pupil such as accommodation disorders (adjustment disorders of the eye), dry mouth or a temporary obstruction of the aqueous humor drainage (angle block)
What do I have to consider after a funduscopy?
The pupil-dilating drugs temporarily hinder the eye's ability to accommodate. As a result, you can see blurred for a while and are slightly dazzled. It is therefore not allowed to drive again until several hours after the funduscopy.
Tags: nourishment organ systems prevention
















.jpg)


.jpg)