Osteoarthritis of the knee
Ricarda Schwarz studied medicine in Würzburg, where she also completed her doctorate. After a wide range of tasks in practical medical training (PJ) in Flensburg, Hamburg and New Zealand, she is now working in neuroradiology and radiology at the Tübingen University Hospital.
More about the experts All content is checked by medical journalists.Doctors describe joint wear in the knee as gonarthrosis. Most of the time there is no specific trigger for this: the knee joints were simply too stressed. Osteoarthritis of the knee can cause knee pain. These can be treated with medication, exercises or surgery. Here you can read everything you need to know about osteoarthritis of the knee.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M17
Gonarthrosis: where does it arise?
Gonarthrosis is wear and tear of the joint (arthrosis) in the knee: the articular cartilage wears out. Later on, neighboring joint areas such as bone parts are also damaged.
Osteoarthritis always forms between two parts of the bone. The knee joint is made up of three bones:
- Thigh bone (femur)
- Kneecap (patella)
- Shin (tibia)
There is a joint connection between each of these bones. With its middle (medial) and lateral (lateral) parts, the shinbone even forms two articulations with the thigh. In technical terms, this is called the different compartments in the knee.
Osteoarthritis forms in the knee
Osteoarthritis of the knee can affect one or more parts (compartments) of the knee joint:
- Gonarthrosis in 1 compartment (unicompartmental gonarthrosis): It exists either between the kneecap and the femur or between the shin and the femur.
- Gonarthrosis in 2 compartments (bicompartmental gonarthrosis): Here, the arthrosis affects the shin and thigh bones.
- Gonarthrosis in 3 compartments (tricompartmental gonarthrosis or pangonarthrosis): The joint wear affects all three parts of the knee joint.
The division into uni-, bi- and tricompartmental osteoarthritis of the knee is important if the joint wear is to be operated on.
Medial and lateral gonarthrosis
If the inner part of the knee joint is affected by wear, there is medial osteoarthritis of the knee. If there is knee osteoarthritis in the outer area, it is called lateral osteoarthritis of the knee.
Activated osteoarthritis of the knee
A worn joint can easily become infected. Parts of the cartilage peel off, cells perish. They collect in the synovial fluid and attract inflammatory cells. A simple osteoarthritis of the knee becomes an activated osteoarthritis of the knee. The knee joint and the surrounding tissue can swell painfully. The activated osteoarthritis of the knee can regress to non-inflamed osteoarthritis in the knee joint if the therapy is correct.
Gonarthrosis: symptoms
Knee wear and tear doesn't always cause discomfort (such as pain); if so, it is referred to as symptomatic osteoarthritis of the knee.
Those affected report knee pain, for example when climbing stairs. With advanced osteoarthritis of the knee, permanent pain can also occur. The knee joint is less mobile. Unsteady gait can arise.
In many patients, knee pain is also dependent on the weather: it becomes worse in cold or wet weather, for example. Those affected then report "sensitivity to the weather".
You can find more about possible symptoms of osteoarthritis of the knee (and other forms of osteoarthritis) in the article Osteoarthritis Symptoms.
Gonarthrosis: frequency
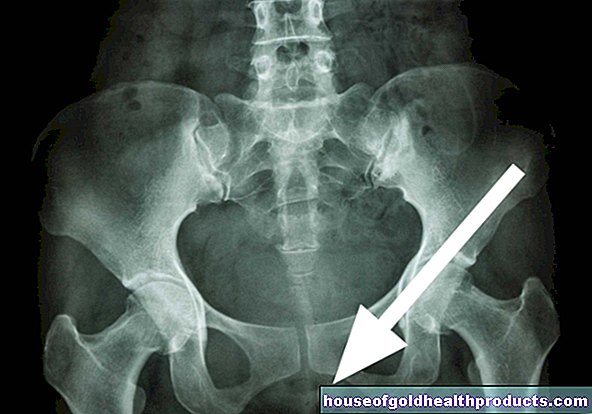
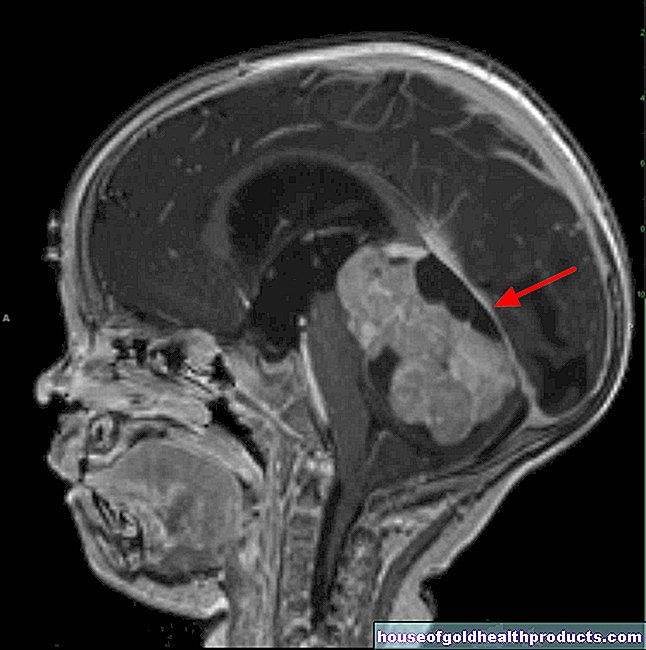
Knee joint osteoarthritis is the most common form of osteoarthritis in Germany. However, the information on frequency fluctuates greatly. The reason is that there are no standardized examination criteria for osteoarthritis of the knee. Most diagnoses are based on the radiological signs of osteoarthritis. These are indications of joint wear in the X-ray, in computed tomography or magnetic resonance tomography.
The likelihood of knee osteoarthritis increases with age. Men are more often affected before the age of 45. Later, more women develop osteoarthritis of the knee.
Gonarthrosis: diagnosis
If osteoarthritis of the knee is suspected, the doctor will first ask the patient to describe their symptoms in detail. He also asks about any injuries or illnesses that currently exist or have occurred in the past. For example, meniscus damage or joint inflammation (arthritis) can promote osteoarthritis of the knee.
In the next step, the doctor will examine the knee joint and check its mobility. An X-ray examination and other imaging procedures help clarify gonarthrosis.
How exactly osteoarthritis of the knee (and other forms of osteoarthritis) is diagnosed can be found in the article osteoarthritis.
Gonarthrosis: therapy
Some general therapeutic measures apply to osteoarthritis of the knee and other forms of osteoarthritis. This includes, for example, relieving the affected joint, but still moving it regularly.
Heat applications such as heating pads or baths help against chronic osteoarthritis pain. Acute complaints, on the other hand, can be relieved more with cold applications such as ice packs. If necessary, medication for the pain is also prescribed.
You can find out more about general therapeutic measures for osteoarthritis of the knee and other forms of osteoarthritis in the article on osteoarthritis.
Gonarthrosis exercises
To stop the disease from progressing, people with osteoarthritis should do knee exercises. These aim to strengthen the muscles on the knee. In this way, you can better absorb stress, which relieves the cartilage in the knee joint.
Caution: The exercises must not cause additional damage to the already damaged knee joint! Therefore, the body weight should not rest on the knee during training. Water aerobics and cycling are therefore particularly suitable.
Special equipment training for people with osteoarthritis is also useful. However, knee exercises must always be discussed with a trained physiotherapist and must not be selected independently.
Gonarthrosis therapy: surgery without joint replacement
In the case of osteoarthritis of the knee, it can be helpful to rinse the joint (lavage). In addition, rough cartilage surfaces in the joint can be smoothed (debridement). Both interventions are carried out as part of an arthroscopy.
Corrective osteotomy is another option for osteoarthritis of the knee. The bones that make up the joint are positioned differently. This should reduce the stress on the osteoarthritis areas.
You can find out more about lavage, debridement and corrective osteotomy in the article on osteoarthritis.
Gonarthrosis therapy: surgery with joint replacement
Sometimes knee complaints in people with osteoarthritis cannot be adequately alleviated by conservative measures or joint-preserving interventions. In the case of severe osteoarthritis of the knee, the affected knee joint is sometimes replaced with a prosthesis:
If the knee osteoarthritis affects only one compartment, a unicompartmental endoprosthesis can be used. In the case of osteoarthritis of the knee in several compartments, a total endoprosthesis can be considered.
Uni-compartment endoprosthesis
A so-called unicondylar prosthesis is primarily used to treat moderate lateral or medial osteoarthritis of the knee. The partial denture only replaces the articular surface. The joint continues to be guided through the capsule and ligament apparatus. Such a partial prosthesis is also referred to as a sled prosthesis.
Patients with a partial prosthesis often judge the functionality of the joint replacement better than people with a total endoprosthesis. In addition, they are usually more satisfied with the outcome of the operation. However, a sled prosthesis is not an option for every patient. If one of the following points applies, the person concerned is more likely to have a total endoprosthesis:
- Age over 65 years
- Gonarthrosis of the kneecap
- Damage (lesion) to the joint capsule or ligaments
- relevant joint misalignments of more than 10 degrees
Total endoprosthesis
There are different forms of total endoprosthesis that can be used for osteoarthritis of the knee. Among other things, they differ in terms of material, structure and anchoring.
Younger patients are more likely to receive cementless prostheses. These can only be attached to a stable bone. If necessary, they can be exchanged relatively easily.
In older patients, prostheses are more likely to be cemented. The reason: The bone structure is often loosened in them, and any other anchoring would be less stable.
There are two groups of total endoprostheses in osteoarthritis of the knee:
- the uncoupled resurfacing
- the axis-guided prosthesis
Unlinked resurfacing
With uncoupled resurfacing, only the joint surfaces are prosthetically treated. There is no fixed connection between the prosthesis parts on the thigh and the tibia. In some cases, a so-called inlay is placed between these two parts of the prosthesis. This keeps the knee joint easy to move.
The prerequisite for this form of total endoprosthesis is that the natural capsule-ligament apparatus is sufficiently stable. Otherwise an axis-guided prosthesis should be used.
Axially guided total endoprostheses
Axial total endoprostheses are used for severe osteoarthritis of the knee with defective ligaments. They have a firm connection between the two parts of the prosthesis on the thigh bone and the tibia. This means that the force no longer has to be held by the capsule or ligaments on the knee. However, the prosthesis is more heavily stressed and can loosen more easily.
Gonarthrosis prosthesis: complications
Knee joint surgery with knee replacement, like all operations, carries general risks. These include, for example, bleeding or infection.
In addition, the inserted prosthesis can loosen over time. Then the operation usually has to be repeated. Sometimes the prosthesis also has to be replaced.
Another danger after the insertion of a prosthesis for osteoarthritis of the knee concerns the kneecap: it can loosen, break or cause pain. In addition, the bony structures around the prosthesis can break. Doctors call this a periprosthetic fracture. Affected osteoarthritis patients have to be operated again.
Additional information
Book recommendations:
- Weak knee: Targeted practice for pain, injuries and osteoarthritis, Kay Bartrow, 2015, TRIAS edition 1.
- Active knee: 100 exercises for osteoarthritis and after joint replacement, injuries, operations, Joachim Merk and Thomas Horstmann, 2013, S. Hirzel Verlag; Edition: 5