Mitochondrial disease
Mareike Müller is a freelance writer in the medical department and assistant doctor for neurosurgery in Düsseldorf. She studied human medicine in Magdeburg and gained a lot of practical medical experience during her stays abroad on four different continents.
More about the experts All content is checked by medical journalists.The term mitochondrial disease describes a disease of certain cell structures, the mitochondria. These are located in every cell in the body and have the task of supplying them with energy. Mitochondrial disease usually occurs in children or early adulthood. Some patients have only mild symptoms, such as muscle weakness on exertion. Others suffer from severe nervous system damage. Read more about the symptoms, diagnosis and therapy of mitochondrial disease here.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. E88G31

Mitochondrial disease: description
What are Mitochondria?
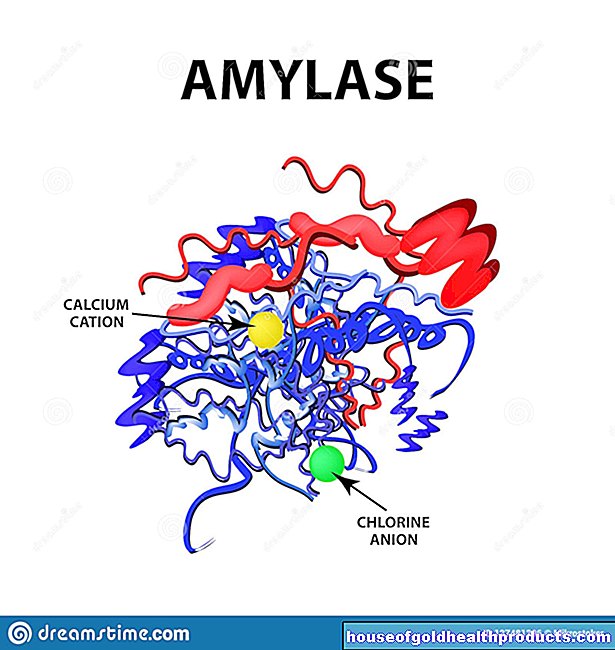
Doctors understand mitochondriopathy to be a disease of certain structures in the body's cells, the mitochondria. These tiny "cell organelles" are also known as the "power plants of the cell". They are found in almost all human cells. Metabolic processes such as the so-called respiratory chain take place in them. Through this process, the body gains around 90 percent of the body's energy from, for example, sugar (glucose) or fatty acids.
In mitochondrial disease, the proteins that are involved in the respiratory chain are not functional. Therefore, only relatively little energy is obtained. The reason for this is a change in the genetic make-up (mutation). This especially affects organs that need a lot of energy. These include the brain or the eye muscles.
Occurrence and frequency
The first symptoms of mitochondrial disease appear in children and adolescents, sometimes not until early adulthood. It is estimated that out of 100,000 people, around 12 have mitochondrial disease.
Mitochondrial disease: symptoms
There are different forms of mitochondrial disease, which differ in their symptoms. According to the symptoms, mitochondrial diseases are divided into different syndromes. The word syndrome describes signs of illness that occur simultaneously and are related.
Common symptoms common to patients with various mitochondrial disorders are:
- Short stature
- Exercise-related muscle weakness
- Eye muscle paralysis
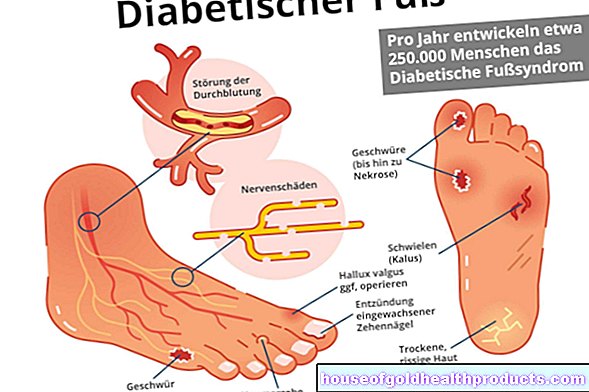
- Diabetes mellitus
- Seizures (epilepsy)
The following syndromes are only a part of possible mitochondrial disease, but other syndromes are less common:
MELAS syndrome
The abbreviation "MELAS" stands for mitochondrial encephalopathy, lactic acidosis and stroke-like episodes. In MELAS syndrome, patients suffer from seizures and dementia. Encephalopathy describes diseases of the brain. Lactic acidosis occurs when the body has to provide a lot of energy without the mitochondrial respiratory chain working. It is the cause of the stroke-like episodes that, like a real stroke, are associated with symptoms of paralysis. The reason is reduced blood flow and a lack of oxygen in the brain. These symptoms usually go away once the lactic acidosis is treated.
MERRF syndrome
The abbreviation “MERRF” stands for myoclonus epilepsy with “ragged red fibers”. Medical professionals refer to an involuntarily twitching musculature as myoclonus. "Red-Ragged-Fibers" describe muscle cells with swollen mitochondria, which the pathologist finds in a tissue sample under the microscope in mitochondrial disease of this type. The patients often suffer from movement and balance disorders, usually severe epilepsy is the main symptom.
Kearns-Syre Syndrome
With this form of mitochondrial disease, the patients primarily suffer from eye damage such as paralysis of the eye muscles or changes in the retina. Heart muscle damage is also common. Regular examinations by a cardiologist are important for these patients. In many of those affected, the hormonal balance is disturbed, which manifests itself in the form of diseases such as diabetes mellitus or an underactive thyroid.
LHON
The abbreviation "LHON" stands for Leber's hereditary optic neuropathy - a disease of the optic nerve (optic nerve).
Mitochondrial disease: causes and risk factors
Changes in the mitochondrion as the cause
In mitochondrial disease, the so-called respiratory chain of the mitochondria is changed. It consists of various proteins and serves as the body's main supplier of energy. The genetic material contains information on how these proteins should be formed and function. If damage occurs there (mutations), the proteins are not produced at all or are built incorrectly. The respiratory chain then does not work properly and the supply of energy is disturbed. Accordingly, the effects of mitochondrial disease mainly affect organs that require a lot of energy. These include, for example, the brain, the eye muscles or the skeletal muscles.
How changes come about
Mitochondrial disease can be inherited or it can develop sporadically without a hereditary predisposition. Usually there is a sporadic change in mitochondrial disease. If they are inherited, the mutation usually comes from the mother. Since the father's sperm leaves its mitochondria behind when the egg cell is fertilized, all of the child's mitochondria later come from the egg cell.
In addition, an egg cell contains mitochondria with various genetic information that can only partially mutate (heteroplasmia). Depending on how many mitochondria of the egg cell were changed and in which organs they occur in the child, the corresponding symptoms and organ involvement appear.
Mitochondrial disease: examinations and diagnosis
Mitochondrial Disease: First Steps to Diagnosis
In order to diagnose “mitochondriopathy”, your doctor will first ask you in detail about your medical history (anamnesis). He will ask you the following questions, among others:
- When did the symptoms first appear?
- Are the discomforts worse when you exercise?
- Are you experiencing muscle pain?
- Do epileptic seizures occur?
- Do any of your family members have similar symptoms?
- Are there any hereditary diseases in your family?
Further examinations are only carried out if the symptoms confirm the suspicion of mitochondrial disease. These should take place in specialized centers.
With the help of blood tests, metabolic products such as milk sugar (lactate) are determined. If there is a suspicion that certain organs are affected by mitochondrial disease, the doctor can order an electrocardiogram (EKG) or a heart echocardiogram (heart ultrasound). The ophthalmologist will do an eye test and assess the fundus. Magnetic resonance imaging (MRI) can be used to detect damage to the brain.
In the further course, the concentrations of the hormones in the body should be determined regularly, since hormonal diseases such as diabetes mellitus or hyperparathyroidism (disease of the parathyroid glands) occur more frequently in patients with mitochondrial disease.
A muscle biopsy provides information
The doctor can safely diagnose mitochondrial disease by taking a tissue sample from a muscle (muscle biopsy) under local anesthesia. A pathologist then examines the sample under a microscope. In addition, experts can analyze the genetic material (DNA) of muscle cells and track down the mutation.
Let us advise you!
Families of those affected should visit a human genetic counseling center after the diagnosis has been completed. There the exact mutation is determined and a family tree is drawn up. In this way, other affected persons can be identified and the risk for possible offspring can be assessed.
Mitochondrial disease: treatment
There is no cure for mitochondrial disease. The aim of treatment is to alleviate the symptoms and prevent possible complications (symptomatic therapy). The doctor adjusts the treatment depending on which syndrome the patient suffers from and which complaints are in the foreground.
Drug treatment options
Some drugs support the work of the respiratory chain in the mitochondria, such as so-called co-factors, antioxidants, vitamin B1 or vitamin B2. Other drugs (anticonvulsants) work against seizures (epilepsy) and in many cases prevent the seizure from occurring again. For example, carbamazepine or lamotrigine are helpful; Valproate must be avoided because of the severe side effects associated with mitochondrial disease. If movement disorders occur, the doctor can administer dopamine in the case of muscle stiffness or botulinum toxin in the case of increased muscle activity. Stroke-like episodes are usually treated with cortisone.
Other treatment options
Endurance sports such as running or cycling are particularly helpful. It is important that patients with mitochondrial disease stay below their maximum exercise limit while exercising.
A high-fat and low-carbohydrate diet (ketogenic) can also help stabilize epilepsy. In doing so, the person concerned must consume enough calories. The patient first learns the ketogenic diet in the hospital, as the ratio of fats to carbohydrates must be carefully observed. Later he can continue the diet at home.
Physiotherapy, occupational therapy and speech therapy are used to improve the function of the muscles.
Mitochondrial disease: disease course and prognosis
The first symptoms of mitochondrial disease usually appear in adolescence or early adulthood, depending on the syndrome. But babies can also be affected. The earlier the children become ill, the faster mitochondrial disease usually progresses. In addition, the symptoms are then often more severe than in patients who later become ill. With them, the disease usually progresses more slowly and with milder symptoms. However, rapid and severe courses are also possible in young adults.
There is no cure for mitochondrial disease. The prognosis depends on how early the first symptoms appear, how quickly the disease progresses, and how severe the seizures are. Life expectancy and quality can be improved through optimal therapy. Whether and which therapy helps with mitochondriopathy varies greatly from patient to patient and requires constant care by specialists.
Tags: nourishment vaccinations baby toddler