Polyarteritis nodosa
Astrid Leitner studied veterinary medicine in Vienna. After ten years in veterinary practice and the birth of her daughter, she switched - more by chance - to medical journalism. It quickly became clear that her interest in medical topics and her love of writing were the perfect combination for her. Astrid Leitner lives with daughter, dog and cat in Vienna and Upper Austria.
More about the experts All content is checked by medical journalists.Polyarteritis nodosa (also known as periarteritis nodosa, Kussmaul-Maier disease, PAN) is a very rare disease of the small and medium-sized arteries. Inflammation causes blood vessels to be damaged. The cause is so far unknown. Read here what risk factors there are, what complications occur and how PAN is treated.
ICD codes for this disease: ICD codes are internationally recognized codes for medical diagnoses. They can be found, for example, in doctor's letters or on certificates of incapacity for work. M30

Brief overview
- What is polyarteritis nodosa? Autoimmune disease that causes inflammation of the small and medium-sized arteries. If the blood vessels are blocked by a blood clot, there is a risk of serious complications such as a heart attack or stroke.
- Causes: Unknown
- Risk factors: viral infections such as hepatitis B or C.
- Symptoms: fever, fatigue, weight loss, damage to the skin and internal organs
- Diagnostics: tissue sample (biopsy), vascular examination (arterial angiography)
- Treatment: Cortisone (corticosteroids) and drugs that suppress the immune system (immunosuppressants)
- Prevention: Hepatitis vaccination
What is PAN
Polyarteritis nodosa (Periarteritis nodosa, Panarteritis nodosa, PAN) is a disease associated with inflammation of the small and medium-sized arteries. It can affect numerous organs and cause various complaints. The name "Kussmaul-Maier disease" goes back to the names of the doctors who first described the disease in 1866.
Inflammation of the blood vessels is summarized under the term "vasculitides". This describes a number of inflammatory rheumatic diseases in which the immune system is directed against the body's own substances (autoimmune disease). In vasculitis, the blood vessels are affected, which leads to circulatory disorders. The reason for this is unclear.
In PAN, small and medium-sized arteries are particularly affected: the inflammation affects all layers of the blood vessels' walls and destroys them over time. As a result, bulges (aneurysms) and narrowing of the vessels (stenoses) form. If blood clots (thromboses) form in this area, the tissue behind the inflammatory focus is only poorly supplied with blood and may die.
In principle, polyarteritis nodosa affects every organ, sometimes even several organs at the same time. However, PAN typically mainly leads to damage to the arteries of the gastrointestinal tract, the muscles and the nervous system. If the change occurs in the skin vessels, lined-up inflammatory nodules become visible, usually on the lower legs and forearms. It is characteristic of PAN that the pulmonary vessels are spared.
Without treatment, the disease is life-threatening. With the appropriate therapy, however, most patients live permanently without symptoms.
frequency
PAN is a very rare disease: 1.6 out of a million people develop polyarteritis nodosa each year. PAN diseases associated with hepatitis infections have decreased significantly in recent years. The reason for this is that hepatitis can be treated better and better.
PAN occurs mainly in middle age, and those affected are on average 46 years old at the time of diagnosis. Men get sick about twice as often as women.
Causes and Risk Factors
The cause of PAN has not yet been fully clarified. Doctors assume that several factors interact in the development of the disease.
In around 20 percent of all PAN patients, the doctor finds evidence of a previous infection with the hepatitis B virus, significantly less often also with hepatitis C. As a result of this infection, so-called "immune complexes" (compounds of virus components and antibodies) are formed deposit in the vessel wall of small and medium-sized vessels and trigger inflammation (immune complex vasculitis) there.
The tissue is severely damaged as a result, narrowing or bulging of the vessel walls occurs. If the affected vessel closes completely, the underlying tissue is no longer supplied with blood and dies (infarction).
Other - very rare - triggers for the formation of such immune complexes are the HI virus (HIV) and the parvovirus B19.
Even more rarely, the disease is associated with the use of certain medications or with congenital immunodeficiencies (weakened or lacking immune defense).
In most patients, however, the cause remains unclear. Doctors then speak of idiopathic polyarteritis nodosa (formerly also known as classic PAN or cPAN).
Symptoms
At the beginning of polyarteritis nodosa, unspecific symptoms such as weight loss, fever and fatigue are usually noticeable. Other common complaints are night sweats and loss of appetite. Every third patient complains of joint or muscle pain. Red spots or garland-shaped bluish veins appear on the skin. Those affected usually feel very sick.
The other symptoms depend on which blood vessels are affected and which organs are damaged as a result. Since panarteritis can basically occur anywhere in the body, infarcts are possible in all body regions or organs.
Nervous system: Damage to the nerves causes pain and paralysis. This is the case in 50 to 70 percent of all PAN patients. Signs of a circulatory disorder in the brain are paralysis, speech disorders, dizziness, headaches, vomiting, seizures (epilepsy) or psychoses. If blood vessels in the brain are affected, a stroke may occur.
Muscles and skin: In 50 percent of cases, the muscles and skin are also affected. On the skin, usually small to pea-sized, bluish-reddish lumps (nodules) can be felt in the area of the elbows as well as the lower legs and ankles. These are eponymous for polyarteritis nodosa.
Circulatory disorders can cause severe tissue damage in the affected area (wounds, dying fingers or toes). Another characteristic is a reticulate, light purple discoloration of the skin (livedo racemosa).
Kidney: The kidneys are involved in almost 50 percent of the cases. If the blood vessels in the kidney are damaged, patients often have high blood pressure. Long-term circulatory disorders or a complete occlusion of the renal arteries often lead to a complete loss of function (renal insufficiency).
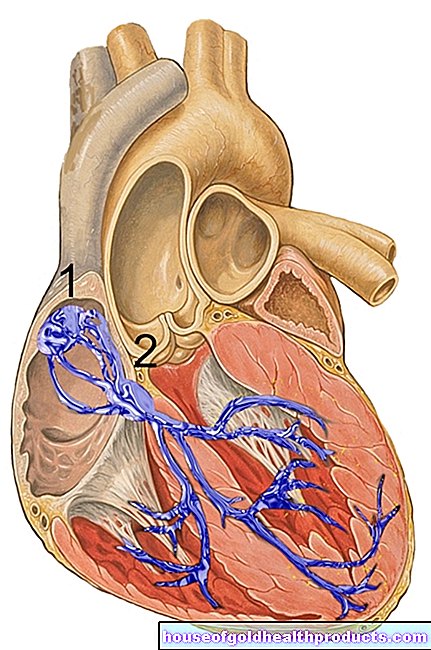
Heart: In the majority of patients, the disease affects the coronary arteries, which supply blood to the heart. Constrictions are noticeable here through complaints such as chest pain or cardiac arrhythmias. A heart attack threatens if it is completely closed.
Gastrointestinal tract: If the PAN affects the gastrointestinal tract, the most common complaints are abdominal pain, diarrhea, bleeding in the intestine or jaundice (jaundice).
Lungs: It is typical of polyarteritis nodosa that the lungs are rarely affected. Blood clots may, however, be washed into the lungs and cause blockage of the pulmonary vessels there (pulmonary infarction, pulmonary embolism).
Reproductive organs: Men with PAN often experience testicular pain.
diagnosis
Polyarteritis nodosa is a very rare disease that causes various symptoms. Because of this, the diagnosis is often made late. The first point of contact if PAN is suspected is the internist or rheumatologist.
In a detailed initial consultation, the doctor asks about the current symptoms (anamnesis) and examines the patient for physical signs of the disease. If periarteritis nodosa is suspected, the doctor will conduct further tests.
These include:
Blood test
In PAN, the blood typically has high levels of inflammation such as an increased rate of sedimentation and an increased CRP value (C-reactive protein). An increased number of white blood cells (leukocytes) and blood platelets (thrombocytes) is also typical, while the blood pigment hemoglobin is low. If organs are affected by polyarteritis nodosa, corresponding changes (e.g. liver values, kidney values) are possible.
In order to rule out or confirm an infection with hepatitis viruses, the doctor has the blood examined for appropriate antibodies.
Examination of the blood vessels (angiography)
With the help of angiography, it is possible to visualize damage to the blood vessels such as bulges or constrictions. To do this, the doctor injects the patient with a contrast medium. The changes become visible during a subsequent X-ray examination. However, the disease cannot be definitively ruled out even if no aneurysms can be seen.
Tissue sample (biopsy)
If there are changes in organs, the doctor will perform a biopsy. He takes a tissue sample from the affected organ and examines it under the microscope for typical changes.
ACR criteria for the classification of polyarteritis nodosa
All of the examinations mentioned give the doctor initial indications that it may be PAN. However, there are no specific tests that enable the doctor to make a clear diagnosis of the disease. If other diseases that cause similar symptoms (such as rheumatoid arthritis or systemic lupus erythematosus) are excluded, the suspicion of PAN is reinforced.
Based on the so-called ACR criteria (named after the American College of Rheumatology), the doctor further narrows the diagnosis PAN. To do this, he analyzes ten criteria that speak in favor of PAN. If three of these ten criteria apply, the diagnosis of polyarteritis nodosa is at least very likely.
- Weight loss of more than four kilograms since the onset of the disease, which is not due to other diseases
- Typical changes in the skin (livedo racemosa)
- Testicular pain or swelling of unknown cause
- Muscle pain (myalgia), heaviness in the legs
- Nerve pain
- Diastolic blood pressure increase> 90 mm Hg
- Serum creatinine increase> 1.5 mg / dl
- Hepatitis virus detection in serum
- Abnormalities in the angiogram (aneurysm, occlusions)
- Typical changes in the tissue sample (biopsy)
treatment
How polyarteritis nodosa is treated depends on which organ is affected.
In acute illness, therapy is initially carried out with high-dose cortisone (has a strong anti-inflammatory effect) and so-called immunosuppressants such as cyclophosphamide. They slow down the excessively working immune system. In severe cases, plasma exchange treatment is sometimes necessary. The immune complexes are filtered out of the patient's blood.
After acute therapy, patients receive milder drugs such as azathioprine or methotrexate (MTX), which also suppress the excessive immune system.
If there is a simultaneous infection with hepatitis viruses, the patients receive low-dose cortisone and antivirals such as interferon-alpha, vidarabine, lamivudine or famciclovir to inhibit the virus from multiplying.
ACE inhibitors are usually used for the high blood pressure that often occurs in polyarteritis nodosa.
forecast
Without treatment, polyarteritis nodosa is usually difficult and the prognosis in these cases is poor.
With appropriate therapy, the prognosis has improved significantly in recent years. While the disease was mostly fatal until around 25 years ago, the survival rate after five years is currently around 90 percent. The prognosis of PAN depends primarily on which organ is affected. If the kidneys, heart, gastrointestinal tract or the nervous system are affected, the prognosis is slightly worse.
In general, the earlier PAN is diagnosed and treated, the easier it is to prevent organ damage. In many cases, the symptoms go away completely.
Prevent
Since the causes of polyarteritis nodosa are not fully understood, no specific prevention is possible. However, vaccination against hepatitis B can reduce the risk of developing PAN.
Tags: travel medicine baby toddler symptoms















.jpg)